Polysaccharide encapsulated bacteria
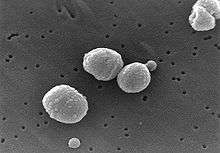
Polysaccharide encapsulated bacteria, frequently referred to simply as encapsulated bacteria and less precisely called encapsulated organisms, are a group of bacteria that have an outer covering, a bacterial capsule, made of polysaccharide.
Examples of encapsulated bacteria
- Hemophilus influenzae type b (Hib)[1]
- Streptococcus pneumoniae (pneumococcus)[1]
- Neisseria meningitidis (meningococcus)[1]
- Group B streptococcus (GBS)[1]
- Klebsiella pneumoniae
- Salmonella typhi[2]
A popular mnemonic to remember most of the encapsulated bacteria is the SHiNE SKiS bacteria (S. pneumo, Hib, N. meningitidis, E. Coli, Salmonella, Klebsiella, Group B Strep).
Role in disease
Many encapsulated bacteria are pathogens that lead to a significant amount of morbidity and mortality.[3] Encapsulated bacteria are antiphagocytic and hence are susceptible to antibody mediated immune response (B cells) as opposed to cell mediated immune response. Patients with B cell deficiencies are highly susceptible to encapsulated bacterial infections.
Asplenia
People that lack a spleen, functionally (as in sickle cell disease[4][5]) or anatomically (due to a splenectomy or congenital absence, as in Ivemark Syndrome for example), have been shown to be more susceptible to these pathogens due to impaired opsonization of such organisms.[6] Therefore, it is standard medical practice to recommend vaccination.
It is generally recommended that people with asplenia are vaccinated against Neisseria meningitidis, Haemophilus influenzae, and Streptococcus pneumoniae.[6] These vaccines can be remembered with the mnemonic: SHiN. Alternatively they can be called the NHS bacteria, as in National Health Service in the UK.
Children
Young children do not have the ability to make antibodies to polysaccharides and are, therefore, more susceptible to encapsulated bacteria, the capsules of which contain polysaccharides. This is especially true for children between six months and one year old (who are typically not breastfed); in these children the maternal antibodies are depleted and endogenous synthesis is not perfected yet due to a poor T-cell independent response. Conjugate vaccines are used to produce an immune response in these cases.
Complement deficiency
Patients with complement deficiency are at risk of infections with encapsulated organisms. There are several types of complement deficiency, two of note are C3 and C5,6,7,8,9. A C3 deficiency allows for infection by encapsulated organisms. A C5,6,7,8,9 (the membrane attack complex) deficiency lead to unopposed Neisseria infections.[7] Vaccination is essential in such patients.
See also
References
- 1 2 3 4 Jakobsen H, Jonsdottir I (2003). "Mucosal vaccination against encapsulated respiratory bacteria--new potentials for conjugate vaccines?". Scand J Immunol. 58 (2): 119–28. doi:10.1046/j.1365-3083.2003.01292.x. PMID 12869132.
- ↑ Lee CJ, Lee LH, Koizumi K. (2002) Polysaccharide Vaccines for Prevention of Encapsulated Bacterial Infections: Part 1. Infect Med 19(3) 127-133. Partial Free Text.
- ↑ Vinuesa C, de Lucas C, Cook M (2001). "Clinical implications of the specialised B cell response to polysaccharide encapsulated pathogens". Postgrad Med J. 77 (911): 562–9. doi:10.1136/pmj.77.911.562. PMC 1757924
 . PMID 11524513. Full Free Text.
. PMID 11524513. Full Free Text. - ↑ Pearson H (1977). "Sickle cell anemia and severe infections due to encapsulated bacteria". J Infect Dis. 136 Suppl: S25–30. doi:10.1093/infdis/136.Supplement.S25. PMID 330779.
- ↑ Wong W, Powars D, Chan L, Hiti A, Johnson C, Overturf G (1992). "Polysaccharide encapsulated bacterial infection in sickle cell anemia: a thirty year epidemiologic experience". Am J Hematol. 39 (3): 176–82. doi:10.1002/ajh.2830390305. PMID 1546714.
- 1 2 Brigden, M. L. (2001). "Detection, education and management of the asplenic or hyposplenic patient". American family physician. 63 (3): 499–506, 508. PMID 11272299.
- ↑ Essential Revision Notes for the MRCP, Philip A Karla, PASTEST.