Varicocele
| Varicocele | |
|---|---|
|
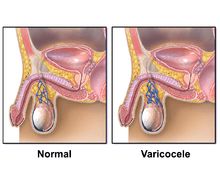
Cross section showing the pampiniform venus plexus | |
| Classification and external resources | |
| Pronunciation | /ˈværᵻkoʊˌsiːl, -kə-/[1][2] |
| Specialty | Urology |
| ICD-10 | I86.1 |
| ICD-9-CM | 456.4 |
| DiseasesDB | 13731 |
| MedlinePlus | 001284 |
| eMedicine | radio/739 |
| Patient UK | Varicocele |
| MeSH | D014646 |
A varicocele is an abnormal enlargement of the pampiniform venous plexus in the scrotum. This plexus of veins drains the testicles. The testicular blood vessels originate in the abdomen and course down through the inguinal canal as part of the spermatic cord on their way to the testis. Upward flow of blood in the veins is ensured by small one-way valves that prevent backflow. Defective valves, or compression of the vein by a nearby structure, can cause dilation of the testicular veins near the testis, leading to the formation of a varicocele. Causes of varicocele include valvular incompetence, Nutcracker syndrome, and renal cell carcinoma. Varicoceles occur in 20% of all men.[3]
Signs and symptoms

Symptoms of a varicocele may include:
- Visible or palpable (able to be felt) enlarged vein[4]
- Dragging-like or aching pain within scrotum
- Feeling of heaviness in the testicle(s)
- Atrophy (shrinking) of the testicle(s)
- Alteration of testosterone levels[5][6][7][8][9][10][11][12][13][14]
- Benign prostatic hyperplasia (BPH) and related urinary problems [15]
Cause
The idiopathic varicocele occurs when the valves within the veins along the spermatic cord do not work properly. This results in backflow of blood into the pampiniform venous plexus. Venous backflow increases vein diameter because of excessive pressure, and testosterone pooling. Pooled blood is toxic and may cause damage to the testicles and veins. Varicoceles develop slowly and may not have any symptoms. They are most frequently diagnosed when a patient is 13–30 years of age. They occur in 20% of all males.[3]
A majority of idiopathic varicoceles occur on the left side,[16] because the left testicular vein travels superiorly and connects to the left renal vein (at a 90-degree angle), while the right testicular vein drains directly into the inferior vena cava. Isolated right sided varicoceles are rare.
A secondary varicocele is due to compression of the venous drainage of the testicle. A pelvic or abdominal malignancy is a definite concern when a unilateral right-sided varicocele is newly diagnosed in a patient older than 40 years of age. One non-malignant cause of a secondary varicocele is the so-called "Nutcracker syndrome", a condition in which the superior mesenteric artery compresses the left renal vein, causing increased pressures there to be transmitted retrograde into the left pampiniform plexus.[17] The most common cause is renal cell carcinoma (a.k.a. hypernephroma) followed by retroperitoneal fibrosis or adhesions.
Lifestyle
Lifestyle factors such as activity type, diet,[18] bowel health,[19] testicular temperature,[20] smoking,[21] and alcohol moderation[18] can affect both the occurrence rate and varicocele symptoms severity.[22]
Pathophysiology
The term varicocele specifically refers to dilatation and tortuosity of the pampiniform plexus, which is the network of veins that drain the testicle. This plexus travels along the posterior portion of the testicle with the epididymis and vas deferens, and then into the spermatic cord. This network of veins coalesces into the gonadal, or testicular, vein. The right gonadal vein drains into the inferior vena cava, while the left gonadal vein drains into the left renal vein at right angle to the renal vein, which then drains into the inferior vena cava. One of the main functions of the plexus is to lower the temperature of the testicles; varicocele causes this function to be lost, hence the most common complication of untreated varicocele is higher temperature of the testes, resulting in testicular atrophy causing infertility.[23]
The small vessels of the pampiniform plexus normally range from 0.5–1.5 mm in diameter. Dilation of these vessels greater than 2 mm is called a varicocele.[24]
Recent studies have shown that the detrimental effect of varicocele on sperm production is progressive and due to reduction in supply of oxygenated blood and nutrient material to the sperm production sites, which persistently reduces the quality and the quantity of the sperms, leading to reduction in their fertility capacity with time.
Blood from the testes that cannot drain via the pampiniform plexus may route through the prostate in a process known as communicating vessels.[15] The increased flow of blood to the prostate can lead to congestion and enlargement of the gland (BPH) both through physical mechanisms and as a result of "accelerated prostate cell proliferation [growth] resulting from the extremely high concentration of free testosterone reaching directly from the testes to the prostate".[15]
Diagnosis

Upon palpation of the scrotum, a non-tender, twisted mass along the spermatic cord is felt. Palpating a varicocele can be likened to feeling a bag of worms.[25] When one is lying down, gravity may allow the drainage of the pampiniform plexus and thus make the mass not obvious.[25] This is especially true in primary varicocele, and absence may be a sign for clinical concern.[25] The testicle on the side of the varicocele may or may not be smaller compared to the other side.
Varicocele can be reliably diagnosed with ultrasound,[26][27] which will show dilation of the vessels of the pampiniform plexus to greater than 2 mm. The patient being studied should undergo a provocative maneuver, such as Valsalva's maneuver (attempting expiration against a closed airway) or standing up during the exam, both of which are designed to increase intra-abdominal venous pressure and increase the dilatation of the veins. Doppler ultrasound is a technique of measuring the speed at which blood is flowing in a vessel. An ultrasound machine that has a Doppler mode can see blood reverse direction in a varicocele with a Valsalva, increasing the sensitivity of the examination.
Treatment
A 2012 Cochrane review found tentative but unclear evidence of improved fertility among males treated for varicocele.[28] The benefit may be as large as one per seven men treated.[29]
Surgery

There is tentative evidence that varicocele surgery may improve fertility in those with obvious findings and abnormal sperm.[30] Prior research found an unclear effect on spontaneous pregnancy rates.[31]
The surgery is performed on an outpatient basis.[32] The three most common approaches are inguinal (groin using percutaneous embolization), retroperitoneal (abdominal using laparoscopic surgery), and infrainguinal/subinguinal (below the groin). Various other techniques may be used. Ice packs should be kept to the area for the first 2 days after surgery to reduce swelling. The patient may be advised to wear a scrotal support for some time after surgery.
Possible complications of this procedure include hematoma (bleeding into tissues), hydrocele (accumulation of fluid around the affected testicle), infection, or injury to the scrotal tissue or structures. In addition, injury to the artery that supplies the testicle may occur.
Couples who are infertile secondary to nonobstructive azoospermia and concurrent varicocele, may benefit from proceeding directly to microsurgical testicular sperm extraction (microTESE) and deferring varicocele repair.[33]
A varicocele can reduce testosterone production in both testies due to increased temperature from the great volume of backed up blood in the varicocele veins. Leydig cells' ability to produce testosterone is reduced in individuals with varicocele. Some studies have shown increases in blood testosterone levels in individuals that have undergone varicocele repair.[34][35]
Embolization
An alternative to surgery is embolization,[36] a minimally invasive treatment for varicocele that is performed by an interventional radiologist. This involves passing a small wire through a peripheral vein and into the abdominal veins that drain the testes. Through a small flexible catheter, the doctor can obstruct the gonadal vein so that the increased pressures from the abdomen are no longer transmitted to the testicles. The obstruction is often performed with many small metal coils. The testicles then drain through smaller collateral veins. The recovery period is significantly less than with surgery and the risk of complications is minimized with overall effectiveness similar to surgery, yet with fewer recurrence rates. However, radiation exposure to the testicles can often not be avoided with this technique.
Alternative medicine
Eastern medical strategies like Yoga, tai chi, and qi gong may have positive benefits for varicocele.[18][37]
Prognosis
Varicocele can be harmless, but in some cases it can cause infertility and pain. Although there are studies showing improvement in sperm quality in 57%,[38] there are also studies showing that the regular surgery has no significant effect on infertility. Thus the surgery may not improve fertility and the patient will need to undergo a nonsurgical treatment.[39][40]
References
- ↑ "Varicocele". Merriam-Webster Dictionary. Retrieved 2016-01-21.
- ↑ "Varicocele". Oxford Dictionaries. Oxford University Press. Retrieved 2016-01-21.
- 1 2 Agarwal, Ashok; Aitken, Robert John; Alvarez, Juan G (17 March 2012). Studies on Men's Health and Fertility. Springer Science & Business Media. p. 538. ISBN 9781617797750.
- ↑ Urologychannel: Varicoele, retrieved October 21, 2006
- ↑ Chen, Shiou-Sheng; Chen, Li-Kuei (2012). "Risk Factors for Progressive Deterioration of Semen Quality in Patients with Varicocele". Urology. 79 (1): 128–32. doi:10.1016/j.urology.2011.08.063. PMID 22055689.
- ↑ Al-Daghistani, Hala I.; Hamad, Abdul-Wahab R.; Abdel-Dayem, Muna; Al-Swaifi, Mohammad; Abu Zaid, Mohammad (2010). "Evaluation of Serum Testosterone, Progesterone, Seminal Antisperm Antibody, and Fructose Levels among Jordanian Males with a History of Infertility". Biochemistry Research International. 2010: 1–8. doi:10.1155/2010/409640.
- ↑ Cantatore, C; Capuano, P; Cobuzzi, I; Vacca, M; Coretti, F; Falagario, D; Spilotros, M; Bettocchi, C; Palumbo, F; Depalo, R (2010). "Semen quality and hormonal levels in infertile patients with varicocele". Archivio italiano di urologia, andrologia. 82 (4): 291–3. PMID 21341585.
- ↑ Mohamad Al-Ali, Badereddin; Marszalek, Martin; Shamloul, Rany; Pummer, Karl; Trummer, Harald (2010). "Clinical Parameters and Semen Analysis in 716 Austrian Patients with Varicocele". Urology. 75 (5): 1069–73. doi:10.1016/j.urology.2009.11.042. PMID 20138656.
- ↑ Sathya Srini, Vasan; Belur Veerachari, Srinivas (2011). "Does Varicocelectomy Improve Gonadal Function in Men with Hypogonadism and Infertility? Analysis of a Prospective Study". International Journal of Endocrinology. 2011: 1–6. doi:10.1155/2011/916380.
- ↑ Li, Fuping; Yue, Huanxun; Yamaguchi, Kohei; Okada, Keisuke; Matsushita, Kei; Ando, Makoto; Chiba, Koji; Fujisawa, Masato (2012). "Effect of surgical repair on testosterone production in infertile men with varicocele: A meta-analysis". International Journal of Urology. 19 (2): 149–54. doi:10.1111/j.1442-2042.2011.02890.x. PMID 22059526.
- ↑ Hsiao, Wayland; Rosoff, James S.; Pale, Joseph R.; Powell, Jonathan L.; Goldstein, Marc (2013). "Varicocelectomy is Associated with Increases in Serum Testosterone Independent of Clinical Grade". Urology. 81 (6): 1213–7. doi:10.1016/j.urology.2013.01.060. PMID 23561709.
- ↑ Tanrikut, Cigdem; Goldstein, Marc; Rosoff, James S.; Lee, Richard K.; Nelson, Christian J.; Mulhall, John P. (2011). "Varicocele as a risk factor for androgen deficiency and effect of repair". BJU International. 108 (9): 1480–4. doi:10.1111/j.1464-410X.2010.10030.x. PMID 21435152.
- ↑ Zohdy, Wael; Ghazi, Sherif; Arafa, Mohamad (2011). "Impact of Varicocelectomy on Gonadal and Erectile Functions in Men with Hypogonadism and Infertility". The Journal of Sexual Medicine. 8 (3): 885–93. doi:10.1111/j.1743-6109.2010.01974.x. PMID 20722780.
- ↑ Luo, De-Yi; Yang, Gang; Liu, Jian-Jun; Yang, Yu-Ru; Dong, Qiang (2010). "Effects of varicocele on testosterone, apoptosis and expression of StAR mRNA in rat Leydig cells". Asian Journal of Andrology. 13 (2): 287–91. doi:10.1038/aja.2010.111. PMC 3739182
 . PMID 21076439.
. PMID 21076439. - 1 2 3 Gat, Yigal; Gornish, M.; Heiblum, M.; Joshua, S. (2008). "Reversal of Benign Prostate Hyperplasia by Selective Occlusion of Impaired Venous Drainage in the Male Reproductive System: Novel Mechanism, New Treatment". First International Journal of Andrologia. 40 (5): 273–281. doi:10.1111/j.1439-0272.2008.00883.x. PMID 18811916.
- ↑ Paduch DA, Skoog SJ (2001). "Current Management of Adolescent Varicocele". PubMed Central (PMC). 3: 120–33. PMC 1476052
 . PMID 16985704.
. PMID 16985704. - ↑ Rudloff, Udo; Holmes, Raymond J.; Prem, Jeffrey T.; Faust, Glenn R.; Moldwin, Robert; Siegel, David (2006). "Mesoaortic Compression of the Left Renal Vein (Nutcracker Syndrome): Case Reports and Review of the Literature". Annals of Vascular Surgery. 20 (1): 120–9. doi:10.1007/s10016-005-5016-8. PMID 16374539.
- 1 2 3 F Yao, David (15 Sep 2015). "Male infertility: lifestyle factors and holistic, complementary, and alternative therapies". Department of Urology, UCLA. 18: 410–8. doi:10.4103/1008-682X.175779. PMC 4854092
 . PMID 26952957. Retrieved 23 March 2016.
. PMID 26952957. Retrieved 23 March 2016. - ↑ Rehman, Khaleeq ur (Nov 24, 2014). "Varicocele and infertility: Role of pressure flow dynamics". wjgnet. Baishideng Publishing Group Inc. Retrieved March 3, 2016.
- ↑ Johnson, A. D. (2012-12-02). Development, anatomy, and physiology. Elsevier. ISBN 9780323143233.
- ↑ Eisenberg, Michael L.; Lipshultz, Larry I. (2011-01-01). "Varicocele-induced infertility: Newer insights into its pathophysiology". Indian Journal of Urology : IJU : Journal of the Urological Society of India. 27 (1): 58–64. doi:10.4103/0970-1591.78428. ISSN 0970-1591. PMC 3114589
 . PMID 21716891.
. PMID 21716891. - ↑ Song, Gook-Sup (2010-04-01). "Could sperm quality be affected by a building environment? A literature review". Building and Environment. 45 (4): 936–943. doi:10.1016/j.buildenv.2009.09.016.
- ↑ Kupis Ł, Dobroński PA, Radziszewski P (2015). "Varicocele as a source of male infertility - current treatment techniques". Cent European J Urol. 68 (3): 365–70. doi:10.5173/ceju.2015.642. PMC 4643713
 . PMID 26568883.
. PMID 26568883. - ↑ Salam, MA (2013). Principles and Practice of Urology. New Delhi 110 002,India: Jaypee Brothers Medical Publishers. p. 752. ISBN 978-93-5025-260-4.
- 1 2 3 Moore, Keith L.; Dalley, Arthur F. (2006). Clinically Oriented Anatomy (5th ed.). Lippincott Williams & Wilkins. p. 228.
- ↑ Bucci, Stefano; Liguori, Giovanni; Amodeo, Antonio; Salamè, Leonardo; Trombetta, Carlo; Belgrano, Emanuele (2007). "Intratesticular varicocele: Evaluation using grey scale and color Doppler ultrasound". World Journal of Urology. 26 (1): 87–9. doi:10.1007/s00345-007-0216-1. PMID 17962950.
- ↑ Charboneau, J. William; Rumack, Carol M; Wilson, Stephanie R. (1998). Diagnostic ultrasound. St. Louis: Mosby. ISBN 0-8151-8683-5.
- ↑ Kroese, AC; de Lange, NM; Collins, J; Evers, JL (17 October 2012). "Surgery or embolization for varicoceles in subfertile men.". The Cochrane database of systematic reviews. 10: CD000479. doi:10.1002/14651858.CD000479.pub5. PMID 23076888.
- ↑ Kroese, A. C. J.; De Lange, N. M.; Collins, J. A.; Evers, J. L. H. (2013). "Varicocele surgery, new evidence". Human Reproduction Update. 19 (4): 317. doi:10.1093/humupd/dmt004. PMID 23515200.
- ↑ Kupis, Ł; Dobroński, PA; Radziszewski, P (2015). "Varicocele as a source of male infertility - current treatment techniques.". Central European journal of urology. 68 (3): 365–70. doi:10.5173/ceju.2015.642. PMC 4643713
 . PMID 26568883.
. PMID 26568883. - ↑ Baazeem, Abdulaziz; Belzile, Eric; Ciampi, Antonio; Dohle, Gert; Jarvi, Keith; Salonia, Andrea; Weidner, Wolfgang; Zini, Armand (2011-10-01). "Varicocele and male factor infertility treatment: a new meta-analysis and review of the role of varicocele repair". European Urology. 60 (4): 796–808. doi:10.1016/j.eururo.2011.06.018. ISSN 1873-7560. PMID 21733620.
- ↑ Hsu, Geng-Long; Ling, Pei-Ying; Hsieh, Cheng-Hsing; Wang, Chii-Jye; Chen, Cheng-Wen; Wen, Hsien-Sheng; Huang, Hsiu-Mei; Einhorn, E. Ferdinand; Tseng, Guo-Fang (2005). "Outpatient varicocelectomy performed under local anesthesia". Asian Journal of Andrology. 7 (4): 439–44. doi:10.1111/j.1745-7262.2005.00080.x. PMID 16281094.
- ↑ Chiles, Kelly A (2016-01-05). "Cost-effectiveness of varicocele surgery in the era of assisted reproductive technology". Asian Journal of Andrology. Asian Journal of Andrology. Retrieved April 7, 2016.
- ↑ Hayden, Russell P.; Tanrikut, Cigdem (2016-05-01). "Testosterone and Varicocele". The Urologic Clinics of North America. 43 (2): 223–232. doi:10.1016/j.ucl.2016.01.009. ISSN 1558-318X. PMID 27132580.
- ↑ Dabaja, Ali; Wosnitzer, Matthew; Goldstein, Marc (2013-08-01). "Varicocele and hypogonadism". Current Urology Reports. 14 (4): 309–314. doi:10.1007/s11934-013-0339-4. ISSN 1534-6285. PMID 23754533.
- ↑ Costanza, M.; Policha, A.; Amankwah, K.; Gahtan, V. (2007). "Treatment of Bleeding Varicose Veins of the Scrotum with Percutaneous Coil Embolization of the Left Spermatic Vein: A Case Report". Vascular and Endovascular Surgery. 41 (1): 73–6. doi:10.1177/1538574406296074. PMID 17277247.
- ↑ Hu, Min; Zhang, Yuehui; Ma, Hongli; Ng, Ernest H. Y.; Wu, Xiao-Ke (2013-07-01). "Eastern medicine approaches to male infertility". Seminars in Reproductive Medicine. 31 (4): 301–310. doi:10.1055/s-0033-1345589. ISSN 1526-4564. PMID 23775386.
- ↑ Mordel, N; Mor-Yosef, S; Margalioth, EJ; Simon, A; Menashe, M; Berger, M; Schenker, JG (1990). "Spermatic vein ligation as treatment for male infertility. Justification by postoperative semen improvement and pregnancy rates". The Journal of reproductive medicine. 35 (2): 123–7. PMID 2406437.
- ↑ Evers, Johannes LH; Collins, John A (2003). "Assessment of efficacy of varicocele repair for male subfertility: A systematic review". The Lancet. 361 (9372): 1849–1852. doi:10.1016/S0140-6736(03)13503-9.
- ↑ Evers, JLH; Collins, JA; Vandekerckhove, P (2001). "Surgery or embolisation for varicocele in subfertile men". Cochrane Database of Systematic Reviews (1): CD000479. doi:10.1002/14651858.CD000479. PMID 11279693.
External links
- Jpost - Israeli Male Fertility Breakthrough Offers Hope To Childless Couples
- Patient UK has a nice patient oriented, but detailed explanation of Varicoceles
- The Royal College of Radiologists has good information on Varicocele Embolisation
