Upper respiratory tract infection
| Upper respiratory tract infection | |
|---|---|
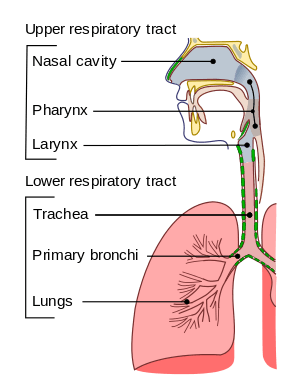 | |
| Conducting passages. | |
| Classification and external resources | |
| Specialty | Infectious disease |
| ICD-10 | J00-06, J30-39 |
| ICD-9-CM | 465.9 |
Upper respiratory tract infections (URI or URTI) are illnesses caused by an acute infection which involves the upper respiratory tract including the nose, sinuses, pharynx or larynx. This commonly includes tonsillitis, pharyngitis, laryngitis, sinusitis, otitis media, and the common cold.[1]
In 2013, 18.8 million cases of upper respiratory infections occurred.[2] As of 2014, upper respiratory infections caused about 3,000 deaths down from 4,000 in 1990.[3]
Classification
- Rhinitis – Inflammation of the nasal mucosa
- Rhinosinusitis or sinusitis – Inflammation of the nose and paranasal sinuses, including frontal, ethmoid, maxillary, and sphenoid
- Nasopharyngitis (rhinopharyngitis or the common cold) – Inflammation of the nares, pharynx, hypopharynx, uvula, and tonsils
- Pharyngitis – Inflammation of the pharynx, hypopharynx, uvula, and tonsils
- Epiglottitis (supraglottitis) – Inflammation of the superior portion of the larynx and supraglottic area
- Laryngitis – Inflammation of the larynx
- Laryngotracheitis – Inflammation of the larynx, trachea, and subglottic area
- Tracheitis – Inflammation of the trachea and subglottic area
Signs and symptoms
Acute upper respiratory tract infections include rhinitis, pharyngitis/tonsillitis and laryngitis often referred to as a common cold, and their complications: sinusitis, ear infection and sometimes bronchitis (though bronchi are generally classified as part of the lower respiratory tract.) Symptoms of URTIs commonly include cough, sore throat, runny nose, nasal congestion, headache, low grade fever, facial pressure and sneezing. Onset of symptoms usually begins 1–3 days after exposure. The illness usually lasts 7–10 days.
Group A beta hemolytic streptococcal pharyngitis/tonsillitis (strep throat) typically presents with a sudden onset of sore throat, pain with swallowing and fever. Strep throat does not usually cause runny nose, voice changes, or cough.
Pain and pressure of the ear caused by a middle ear infection (otitis media) and the reddening of the eye caused by viral conjunctivitis are often associated with upper respiratory infections.
Cause
In one study, 250 patients with the cold were assessed over a period of time, and it was found that the most common cause of the infection was due to the rhinovirus.[4] Other viral causes of upper respiratory infections include the influenza virus, adenovirus, enterovirus, and respiratory syncytial virus.[4]
Up to 15% of acute pharyngitis cases may be caused by bacteria, most commonly Streptococcus pyogenes, a group A streptococcus in streptococcal pharyngitis ("strep throat").[5] Other bacterial causes are Streptococcus pneumoniae, Haemophilus influenzae, Corynebacterium diphtheriae, Bordetella pertussis, and Bacillus anthracis.
Diagnosis
| Symptoms | Allergy | URI | Influenza |
|---|---|---|---|
| Itchy, watery eyes | Common | Rare (conjunctivitis may occur with adenovirus) | Soreness behind eyes, sometimes conjunctivitis |
| Nasal discharge | Common | Common | Common |
| Nasal congestion | Common | Common | Sometimes |
| Sneezing | Very common | Very common | Sometimes |
| Sore throat | Sometimes (postnasal drip) | Very common | Sometimes |
| Cough | Sometimes | Common (mild to moderate, hacking) | Common (dry cough, can be severe) |
| Headache | Uncommon | Rare | Common |
| Fever | Never | Rare in adults, possible in children | Very common (100-102 °F (or higher in young children), lasting 3–4 days; may have chills) |
| Malaise | Sometimes | Sometimes | Very common |
| Fatigue, weakness | Sometimes | Sometimes | Very common, can last for weeks, extreme exhaustion early in course |
| Muscle pain | Never | Slight | Very common, often severe |
Prevention
Probiotics may be useful in preventing URTIs.[6] Vaccination may even help prevent URTIs, mostly against influenza viruses, adenoviruses, measles, rubella, Streptococcus pneumoniae, Haemophilus influenzae, diphtheria, Bacillus anthracis, and Bordetella pertussis.
Treatment

Treatment depends on the underlying cause. There are currently no medications or herbal remedies that have been conclusively demonstrated to shorten the duration of the illness.[7] Treatment comprises symptomatic support usually via analgesics for headache, sore throat and muscle aches.[8]
Moderate exercise in sedentary subjects with naturally acquired URTI probably does not alter the overall severity and duration of the illness.[9] Mild sleep deprivation has been shown to be associated with increased susceptibility to infection.[10][11] No randomized trials have been conducted to ascertain benefits of increasing fluid intake.[12]
Antibiotics
Judicious use of antibiotics can decrease adverse effects of antibiotics as well as decrease costs. Decreased antibiotic usage will also prevent drug resistant bacteria, which is a growing problem in the world. Health authorities have been strongly encouraging physicians to decrease the prescribing of antibiotics to treat common upper respiratory tract infections because antibiotic usage does not significantly reduce recovery time for these viral illnesses.[13] Some have advocated a delayed antibiotic approach to treating URIs which seeks to reduce the consumption of antibiotics while attempting to maintain patient satisfaction. Most studies show no difference in improvement of symptoms between those treated with antibiotics right away and those with delayed prescriptions.[14] Most studies also show no difference in patient satisfaction, patient complications, symptoms between delayed and no antibiotics. A strategy of "no antibiotics" results in even less antibiotic use than a strategy of "delayed antibiotics". However, in certain higher risk patients with underlying lung disease, such as chronic obstructive pulmonary disease (COPD), evidence does exist to support the treatment of bronchitis with antibiotics to shorten the course of the illness and decrease treatment failure.[15]
Decongestants
According to a Cochrane review, single oral dose of nasal decongestant in the common cold is modestly effective for the short term relief of congestion in adults; however, "there is insufficient data on the use of decongestants in children." Therefore, decongestants are not recommended for use in children under 12 years of age with the common cold.[16] Oral decongestants are also contraindicated in patients with hypertension, coronary artery disease, and history of bleeding strokes.[17][18]
Alternative medicine
The use of vitamin C in the inhibition and treatment of upper respiratory infections has been suggested since the initial isolation of vitamin C in the 1930s. Some evidence exists to indicate that it could be justified in persons exposed to brief periods of severe physical exercise and/or cold environments.[19]
The use of nasal irrigation has been shown to alleviate symptoms in some people.[20] There are also saline nasal sprays which can be of benefit.
Epidemiology

In 2013 18.8 billion cases of upper respiratory infections occurred.[2] As of 2014, upper respiratory infections caused about 3,000 deaths down from 4,000 in 1990.[3] In the United States, URIs are the most common infectious illness in the general population. URIs are the leading reasons for people missing work and school. URI is the leading diagnosis in the office setting.[22]
See also
References
- ↑ Eccles MP, Grimshaw JM, Johnston M; et al. (2007). "Applying psychological theories to evidence-based clinical practice: Identifying factors predictive of managing upper respiratory tract infections without antibiotics". Implement Sci. 2: 26. doi:10.1186/1748-5908-2-26. PMC 2042498
 . PMID 17683558.
. PMID 17683558. - 1 2 Global Burden of Disease Study 2013, Collaborators (22 August 2015). "Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013.". Lancet (London, England). 386 (9995): 743–800. doi:10.1016/s0140-6736(15)60692-4. PMID 26063472.
- 1 2 Lozano, R; Naghavi, M; Foreman, K; Lim, S; Shibuya, K; Aboyans, V; Abraham, J; Adair, T; Aggarwal, R; Ahn, SY; Alvarado, M; Anderson, HR; Anderson, LM; Andrews, KG; Atkinson, C; Baddour, LM; Barker-Collo, S; Bartels, DH; Bell, ML; Benjamin, EJ; Bennett, D; Bhalla, K; Bikbov, B; Bin Abdulhak, A; Birbeck, G; Blyth, F; Bolliger, I; Boufous, S; Bucello, C; et al. (15 December 2012). "Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010". Lancet. 380 (9859): 2095–128. doi:10.1016/S0140-6736(12)61728-0. PMID 23245604.
- 1 2 Mika J. Mäkelä; Tuomo Puhakka; Olli Ruuskanen; Maija Leinonen; Pekka Saikku; Marko Kimpimäki; Soile Blomqvist; Timo Hyypiä; Pertti Arstila (1998). "Viruses and Bacteria in the Etiology of the Common Cold". J Clin Microbiol. 36 (2): 539–542. PMC 104573
 . PMID 9466772.
. PMID 9466772. - ↑ Bisno, AL. Acute pharyngitis. N Engl J Med. 2001;344:205.
- ↑ Hao, Q; Lu, Z; Dong, BR; Huang, CQ; Wu, T (7 September 2011). Dong, Bi Rong, ed. "Probiotics for preventing acute upper respiratory tract infections". Cochrane database of systematic reviews (Online). 9 (9): CD006895. doi:10.1002/14651858.CD006895.pub2. PMID 21901706.
- ↑ Smith, SM; Schroeder, K; Fahey, T; Smith, Susan M (2008). Smith, Susan M, ed. "Over-the-counter medications for acute cough in children and adults in ambulatory settings". Cochrane database of systematic reviews (Online) (1): CD001831. doi:10.1002/14651858.CD001831.pub3. PMID 18253996.
- ↑ "Common Cold: Treatments and Drugs". Mayo Clinic. Retrieved 9 January 2010.
- ↑ Weidner T, Schurr T (August 2003). "Effect of exercise on upper respiratory tract infection in sedentary subjects". Br J Sports Med. 37 (4): 304–6. doi:10.1136/bjsm.37.4.304. PMC 1724675
 . PMID 12893713.
. PMID 12893713. - ↑ "Effects of sleep on the production of cytokines in humansPsychosomatic Medicine", Vol 57, Issue 2 97-104
- ↑ Behavioural Brain Research Volume 69, Issues 1-2, July–August 1995, Pages 43-54 The Function of Sleep
- ↑ BMJ. 2004;328:499-500
- ↑ Reveiz L, Cardona AF, Ospina EG (2007). Reveiz L, ed. "Antibiotics for acute laryngitis in adults". Cochrane Database Syst Rev (2): CD004783. doi:10.1002/14651858.CD004783.pub3. PMID 17443555.
- ↑ Spurling GK, Del Mar CB, Dooley L, Foxlee R (2007). Spurling GK, ed. "Delayed antibiotics for respiratory infections". Cochrane Database Syst Rev (3): CD004417. doi:10.1002/14651858.CD004417.pub3. PMID 17636757.
- ↑ Ram FS, Rodriguez-Roisin R, Granados-Navarrete A, Garcia-Aymerich J, Barnes NC (2006). Ram FS, ed. "Antibiotics for exacerbations of chronic obstructive pulmonary disease". Cochrane Database Syst Rev (2): CD004403. doi:10.1002/14651858.CD004403.pub2. PMID 16625602.
- ↑ Spurling GKP, Del Mar C, Dooley L, Foxlee R. Delayed antibiotics for respiratory infections. Cochrane Database of Systematic Reviews 2007, Issue 3. Art. No.: CD004417. doi:10.1002/14651858.CD004417.pub3.
- ↑ Tietze KJ. Disorders related to cold and allergy. In: Berardi RR, ed. Handbook of Nonprescription Drugs. 14th ed. Washington, DC: American Pharmacists Association; 2004:239-269.
- ↑ Common cold. In: Covington TR, ed. Nonprescription Drug Therapy. St Louis, Mo: Facts & Comparisons; 2002:743-769.
- ↑ Douglas RM, Hemilä H, Chalker E, Treacy B (2007). Hemilä H, ed. "Vitamin C for preventing and treating the common cold". Cochrane Database Syst Rev (3): CD000980. doi:10.1002/14651858.CD000980.pub3. PMID 17636648.
- ↑ Kassel, JC; King, D; Spurling, GK (2010-03-17). King, David, ed. "Saline nasal irrigation for acute upper respiratory tract infections". Cochrane database of systematic reviews (Online) (3): CD006821. doi:10.1002/14651858.CD006821.pub2. PMID 20238351.
- ↑ "Mortality and Burden of Disease Estimates for WHO Member States in 2002" (xls). World Health Organization. 2002.
- ↑ 1.Cherry DK, Hing E, Woodwell DA, Rechtsteiner EA. National Ambulatory Medical Care Survey: 2006 Summary. Hyattsville, MD: National Center for Health Statistics; 2008. National health statistics reports.
External links
- Colds and the Flu - Treatment from FamilyDoctor
- Upper Respiratory Tract Infection from Cleveland Clinic Online Medical Reference