Surgical treatment of ingrown toenails



Surgical treatments of ingrown toenails include a number of different options. If conservative treatment of a minor ingrown toenail does not succeed or if the ingrown toenail is severe, surgical management is recommended by a podiatrist.[1] The initial surgical approach is typically a partial avulsion of the nail plate known as a wedge resection or a complete removal of the toenail.[1] If the ingrown toenail reoccurs despite this treatment, destruction of the germinal matrix with phenol is recommended.[1] Antibiotics are not needed if surgery is performed.
Wedge resection
Partial removal of the nail or an offending piece of nail. Here, the digit is first injected with a common local anesthetic. When the area is numb, the physician will perform an onychectomy in which the nail along the edge that is growing into the skin is cut away (ablated) and the offending piece of nail is pulled out. Any infection is surgically drained. This process is referred to as a "wedge resection" or simple surgical ablation and is non-permanent (i.e., the nail will re-grow from the matrix). The entire procedure may be performed in a physician's office and takes approximately thirty to forty-five minutes depending on the extent of the problem. The patient is allowed to go home immediately and the recovery time is anywhere from a two weeks to two months barring any complications such as infection. As a follow-up, a physician may prescribe an oral or topical antibiotic or a special soak to be used for approximately a week after the surgery. Some use "lateral onychoplasty" or "wedge resection" as the method of choice, for ingrown toenails. A wide wedge resection, with a total cleaning of nail matrix, has a nearly 100% success rate. Some physicians will not perform a complete nail avulsion (removal) except under the most extreme circumstances. In most cases, these physicians will remove both sides of a toenail (even if one side is not currently ingrown) and coat the nail matrix on both of those sides with a chemical or acid (usually phenol) to prevent re-growth. This leaves the majority of the nail intact, but ensures that the problem of ingrowth will not re-occur. There are possible disadvantages if the nail matrix is not coated with the applicable chemical or acid (phenol) and is allowed to re-grow; this method is prone to failure. Also, the underlying condition can still become symptomatic as the nail grows out over the course of up to a year: the nail matrix might be manufacturing a nail that is simply too curved, thick, wide or otherwise irregular to allow for normal growth. Furthermore, the flesh can be injured very easily by concussion, tight socks, quick twisting motions while walking or just the fact the nail is growing incorrectly (likely too wide). This hypersensitivity to continued injury can mean chronic ingrowth; the solution is nearly always edge avulsion by the highly successful phenolisation.
Recurrence
If the nail becomes ingrown again after a wedge resection more invasive surgery is required. This can often include the destruction of the nail bed. This surgery takes longer than the minor wedge resection. During it, the toe will be torniqued and incisions will be made from the front of the toe to around 1 cm behind the rear of the visible part of the nail. These incisions are quite deep and will require stitching and will also scar. The nail will then be cut out, much like a wedge resection and the nail bed broken to prevent regrowth. The nail will be significantly narrower after this surgery and may appear visibly deformed but will not become ingrown again. Note: if undertaking this surgery it is advisable to leave at least four days before walking any further than very short distances as even with painkillers this can be exceedingly painful. It is also important if you are required by your employer to stand for extended periods of time that they be made aware you may be unable to work for 1–2 weeks (at most) depending on your speed of recovery.
Avulsion procedure
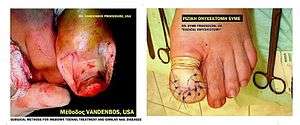
In case of recurrence in spite of complete removal, and if the patient never feels any pain before inflammation occurs, the condition is more likely to be onychia which is often confused for an ingrown or ingrowing nail (onychocryptosis). Complete removal of the whole nail is a simple procedure. Anaesthetic is injected and the nail is removed quickly by pulling it outward from the toe. The patient can function normally immediately after the procedure and most discomfort fades after a few days. The entire procedure can be performed in approximately 20 minutes and is less complex than the wedge resection above. The nail will grow back. However, in most cases it will cause further problems as it can become ingrown very easily as the nail grows outward. It can be easily injured by concussion and in some cases grows back too thickly, too wide or deformed. This procedure can thus result in chronic ingrown nails and is therefore considered a generally unsuccessful solution, especially considering the pain involved. Accordingly, in some cases as determined by a doctor, the nail matrix is coated with a chemical (usually phenol) so none of the nail will ever grow back. This is known as a permanent or full nail avulsion, or full matrixectomy, phenolisation, or full phenol avulsion. As can be seen in the images below, the nail-less toe does not look like a normal toe. Fake nails or nail varnish can still be applied to the area to provide a temporary normal appearance. In a small number of cases phenolisation is not successful and must be repeated, and podiatrists routinely warn patients of this possibility of regrowth.[2]
Vandenbos procedure
The Vandenbos procedure was first described by Vandenbos KQ and Bowers WP in 1959 in the US Armed Forces Medical Journal.[3] They reported on 55 patients and had no recurrences. Subsequently, Dr. Henry Chapeskie performed this procedure on over 1,100 patients with no recurrences since 1988. Unlike other procedures used to treat ingrown toenails, the Vandenbos procedure doesn't touch the nail. In this procedure, the involved toe is first anesthetized with a digital block and a tourniquet applied. An incision is made proximally from the base of the nail about 5 mm (leaving the nail bed intact) then extended toward the side of the toe in an elliptical sweep to end up under the tip of the nail about 3–4 mm in from the edge. It is important that all the skin at the edge of the nail be removed. The excision must be adequate often leaving a soft tissue deficiency measuring 1.5 × 3 cm. A portion of the lateral aspect of the distal phalanx is occasionally exposed without fear of infection. Antibiotics are not necessary as the wound is left open to close by secondary intention. Postoperative management involves soaking of the toe in warm water 3 times/day for 15–20 minutes. The wound is healed by 4–6 weeks. No cases of osteomyelitis have been reported. When healed, the nail fold skin remains low and tight at the side of the nail.
 Ingrown toe before Vandenbos procedure
Ingrown toe before Vandenbos procedure Intraoperative toe during the procedure
Intraoperative toe during the procedure Intraoperative toe during the procedure
Intraoperative toe during the procedure Healed ingrown toe after Vandenbos procedure
Healed ingrown toe after Vandenbos procedure Healed ingrown toe after Vandenbos procedure
Healed ingrown toe after Vandenbos procedure- Ingrown toe before Vandenbos procedure
 Healed ingrown toe after Vandenbos procedure
Healed ingrown toe after Vandenbos procedure
The Syme procedure
In difficult or recurrent cases of Onychocryptosis (Ingrown Toenail) the patient's symptoms persist and he/she asks for a permanent operative solution. The "Avulsion procedure" is a simple method, but surgeon needs to be experienced for a total destruction, or removal of the nail matrix. A second disadvantage is the long term of healing and recovery time(> 2 months). In these cases, the best method is the Syme procedure, that means total nail matrix removal + skin flap transfer + phalanx partial osteotomy + stitching.
Phenolisation

Following injection of a local anaesthetic at the base of the toenail and perhaps application of a tourniquet, the surgeon will remove (ablate) the edge of the nail growing into the flesh and destroy the matrix area with phenol to permanently and selectively ablate the matrix that is manufacturing the ingrown portion of the nail (i.e., the nail margin). This is known as a partial matrixectomy, phenolisation, phenol avulsion or partial nail avulsion with matrix phenolisation. Also, any infection is surgically drained. After this procedure, other suggestions on aftercare will be made, such as salt water bathing of the digit in question. The point of the procedure is that the nail does not grow back where the matrix has been cauterized and so the chances of further ingrowths are very low. The nail is slightly (usually one millimetre or so) narrower than prior to the procedure and is barely noticeable one year later. The surgery is advantageous because it can be performed in the doctor's office under local anaesthesia with minimal pain following the intervention. Also, there is no visible scar on the surgery site and a nominal chance of recurrence. Although the chances of reoccurrence of ingrown nails in an area that has undergone phenolisation are lower than nails who have just had the ingrown nail removed, if the application of the phenol was improperly performed or an insufficient quantity of phenol was applied to the afflicted area; the nail matrix can regenerate from its partial cauterization and grow new nail. This will result in a recurrence of the ingrown nail in approximately 4–6 months as the skin that the original ingrown nail grew under would also recover from the procedure (but the recovery of the skin either side of the nail is standard in this type of procedure) as well as the nail. Many patients who suffer from a minor recurrence of the ingrown nail often have the procedure performed again, with wiser patients asking the doctor to revise the procedure and try to assure that the procedure is performed correctly. However, some patients who suffer a more severe recurrence see a podiatrist who will perform the procedure again or resort to a more drastic and permanent solution (such as removal of the entire nail or the Vandenbos Procedure) if there are multiple recurrences of the ingrown nail.
References
- 1 2 3 Heidelbaugh, JJ; Lee, H (Feb 15, 2009). "Management of the ingrown toenail.". American family physician. 79 (4): 303–8. PMID 19235497.
- ↑ http://www.orthotics-london.com/optimotion.pdf
- ↑ Vandenbos KQ, Bowers WP (1959). "Ingrown toenail: a result of weight bearing on soft tissue". US Armed Forces Medical Journal. 10 (10): 1168–73.
External links
| Wikimedia Commons has media related to Surgical treatment of ingrown toenails. |
- "Ingrown Toenails" Information regarding ingrown toenails and a detailed description of the Vandenbos procedure including pictures, research articles and a video of the procedure
- "Nail Surgery" Chapter 33 of Textbook of Hallux Valgus and Forefoot Surgery,complete text online in PDF file
- "Complete Nail Surgery Photos Photos and comments showing a full nail removal from beginning to end.