Sporothrix schenckii
| Sporothrix schenckii | |
|---|---|
 | |
| Conidiophores and conidia | |
| Scientific classification | |
| Kingdom: | Fungi |
| Division: | Ascomycota |
| Class: | Sordariomycetes |
| Order: | Ophiostomatales |
| Family: | Ophiostomataceae |
| Genus: | Sporothrix |
| Species: | S. schenckii |
| Binomial name | |
| Sporothrix schenckii Hektoen & C.F.Perkins (1900) | |
Sporothrix schenckii is a fungus that can be found world-wide in the environment. The species is present in soil as well as in and on living and decomposing plant material such as peat moss. It can infect humans as well as animals and is the causative agent of sporotrichosis, commonly known as "rose handler's disease".[1] The most common route of infection is the introduction of spores to the body through a cut or puncture wound in the skin. Infection commonly occurs in otherwise healthy individuals but is rarely life-threatening and can be treated with antifungals. In the environment it is found growing as filamentous hyphae. In host tissue it is found as a yeast. The transition between the hyphal and yeast forms is temperature dependent making S. schenckii a thermally dimorphic fungus.[2]
Morphology

Sporothrix schenckii can be found in one of two morphologies, hyphal or yeast. The hyphal form is found in the environment on plants and decaying matter. When the fungus makes the transition into a host, the yeast morphology predominates.
Hyphal
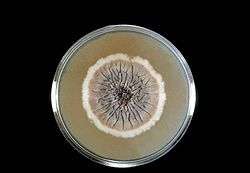
When in the environment or grown in the laboratory at 25 °C (77 °F) S. schenckii assumes its hyphal form.[5] Macroscopically, filaments are apparent and colonies are moist, leathery to velvety, and have a finely wrinkled surface. The colour is white initially and may change color over time to become cream to dark brown (“dirty candle-wax” color).[2] Microscopically, hyphae are septate approximately 1 to 2μm in diameter. Conidia are oval shaped and glass like (hyaline) in appearance. They may be colorless or darkly colored. Conidia are sometimes referred to as resembling a flower.[6]
Yeast
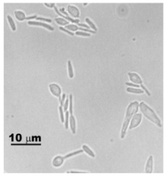
At 37 °C (99 °F) either in the laboratory or in host tissue, S. schenckii assumes its yeast form. Macroscopically, the yeast form grows as smooth white or off-white colonies. Microscopically, yeast cells are 2 to 6μm long and show an elongated cigar-shaped morphology.[2]
Epidemiology and Risk Factors
S. schenckii has a worldwide distribution[2] but certain areas of the world including Peru, have a higher incidence of disease.[7] Based on sequence analysis[8] it has been found that S. schenckii isolates can be placed in phylogenetic groups that reflect the region from which they were isolated. S. schenckii is often isolated from plants and associated packing material.[9] Gardeners,[10] landscapers,[11] and foresters[9] are at high risk of infection. Sporothrix infection can also be transmitted by cat bites or scratches. This mode of transmission has been responsible for epidemics of sporotrichosis.[12] Immunocompromised individuals are at increased risk of infection and such patients often exhibit more severe forms of disease.[13][14][15]
Sporotrichosis

S. schenckii most commonly enters the body through minor trauma that compromises the skin barrier.[13] It is this route of infection, coupled with its presence on roses that give sporotrichosis its common name of "rose-handler's disease"[16] or "rose thorn disease".[17] Inhalation of spores is a rare route of infection largely associated with immunocompromised hosts.[18]
Cutaneous and Lymphocutaneous
The cutaneous form of disease is caused by introduction of S. schenckii into the body through disruption of the skin barrier.[13] The first symptom of cutaneous sporotrichosis is a small skin lesion. These lesions may show ulceration and/or erythema.[2] Commonly, infection spreads through the lymph along lymphatic vessels and causes lymphocutaneous sporotrichosis. This form of disease is characterized by the appearance of lesions at sites distant to the initial infection.[2] Infection can occur in nonhuman animals and may be transmitted to humans through contact. Veterinarians are at particularly high risk of contracting disease from animals (zoonotic infection).[19]
Disseminated
Disseminated disease occurs when the fungus spreads throughout the body. Found only in immunocompromised patients,[2][14][18] it is a very severe condition. When infection becomes disseminated, S. schencki can afflict joints, the brain, and the spine.[2] Patients with this condition must be treated aggressively with antifungals and may remain on prophylactic antifungal drugs for life to prevent recurrence or reinfection.[13]
Diagnostic Tests
Sporothrix infection presents macroscopically with nonspecific symptoms.[20] In the clinical laboratory, many fungi isolated in culture are disregarded as contaminants.[21] Therefore, accurate patient histories are important[1] to establish suspicion of sporotrichosis and to inform which diagnostic tests are required.[2] S. schenckii infection may also be confused with other diseases such as pyoderma gangrenosum[20] or sarcoidosis[22] further underscoring the need for accurate diagnoses.
Primary Cultures
Growing the fungus in pure culture is the most reliable way to identify Sporothrix infection.[1] A patient swab or biopsy is used to inoculate Sabouraud agar[18] or brain heart infusion agar.[16] Sabouraud agar is incubated at room temperature for macroscopic observation of the off-white or dark brown/black hyphal form of the fungus and microscopic examination of hyphae and conidia.[1][18] The yeast form is grown on brain heart infusion agar at 37 °C (99 °F).[16] Observation of yeast colonies in addition to the hyphal form is required to confirm diagnosis of S. schenckii.[20] Growth on media occurs in approximately one to three weeks[16] meaning that results from patient cultures will not be immediately available to make treatment decisions.
Sporotrichin Skin Test
A skin test uses an antigen generated from laboratory grown S. schenckii to challenge the patient's immune system. The antigen is intradermally injected and the test is interpreted 48 hours later. Erythema at the site of injection indicates a positive response.[2][16] The major advantage of this test is its rapidity and ease of use. Although it provides results more quickly than a fungal culture, the sporotrichin skin test has some important limitations. Cross reactions with other fungal species[23] as well as positive reactions in healthy individuals[2] have been observed. In addition, the term "sporotrichin" does not indicate a specific molecule but only any antigen derived from S. schenckii. The specific antigen used in skin testing is not standardized with multiple studies being conducted with widely varying preparations. However, owing to its simplicity, skin testing remains the method of choice for large-scale epidemiological investigations.[2]
Molecular Methods
Molecular diagnostic techniques have been used as rapid, sensitive, and specific tests for the presence of S. schenckii.[24] PCR methods that specifically amplify the ribosomal RNA gene have been shown to detect S. schenckii in clinical samples with minimal interference from host or bacterial sequences.[25] Serum antibody reactivity to S. schenckii antigens can also be quantified by ELISA.[26] Although molecular biology techniques are promising in their use as diagnostic tools, their cost as well as requirement for specialized equipment and expertise means that more traditional diagnostic methods still play an important role in Sporothrix schenckii treatment.
Treatment
Antifungal Drugs
Where available and tolerated by the patient, antifungal drugs are indicated as the primary treatment of sporotrichosis. For cutaneous infection itraconazole or terbinafine are the primary treatment with fluconazole being recommended if primary antifungals are not well-tolerated. When infection is disseminated throughout the body, Amphotericin B is the drug of choice. To completely clear the fungus, the course of treatment generally lasts from 3 to 6 months.[13] In vitro susceptibility to antifungal drugs has been shown to be dependent on the growth phase (hyphal or yeast) of the fungus.[27]
Potassium Iodide
Oral administration of a saturated potassium iodide solution was the first effective treatment for sporotrichosis and remains the drug of choice in many parts of the world owing to its low cost and availability.[28] Although effective, it has since been supplanted by antifungal drugs[13] due to the requirement for multiple daily doses as well side effects including gastrointestinal upset or thyroid imbalance.[28]
Virulence Factors
Melanin Production
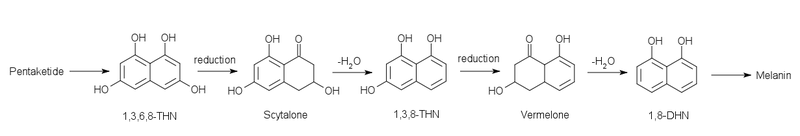
S. schenckii synthesizes melanin both in vitro and in vivo[5] Melanin production is a virulence factor found in many fungi that cause disease[29] and its production in S. schenckii protects the fungus from oxidative stress as well as ultraviolet light and macrophage killing. Melanin has been shown to be synthesized using the 1,8-DHN pentaketide pathway (below).[5]
Adhesins
Adhesion is an important component of pathogenesis. The yeast form of S. schenckii shows an increased ability to bind[2] to the host extracellular matrix proteins fibronectin and laminin using two separate receptors specific for these proteins.[31]
Proteases
S. schenckii breaks down proteins by producing two separate proteases, a serine protease and an aspartic protease.[32] These proteases appear to be essential for fungal growth. However, they have some functional overlap as the inactivation of either protein does not affect growth but inactivation of both inhibits the fungus.[33] Protease activity has been shown to be important in in vivo infection of mice.[32] Substrates for these proteases include the skin proteins type-I collagen, stratum corneum, and elastin.[32]
Heat Tolerance
Growing at host body temperature (37 °C (99 °F)) is an important requirement for pathogenesis. Some strains of S. schenckii are restricted to growing at 35 °C (95 °F) and consequently usually cause disease only on the skin as it is cooler than the body's interior. Those that are capable of growth at body temperature are more often associated with disseminated disease.[32]
Immune Response
Infection by S. schenckii is generally self-limiting in immunocompetent hosts. The immune response prevents fungal dissemination and is the reason that most Sporothrix infections are cutaneous.[34]
Innate
The yeast form of S. schenckii is effectively phagocytosed by cells of the innate immune system[34] and are recognized based on the sugars displayed on their surface[35] or lipids in the yeast cell membrane.[34] Although they are taken up, they are not efficiently killed. It is hypothesized that ergosterol peroxide reacts with and detoxifies reactive oxygen species generated by the respiratory burst used by phagocytes to kill cells they have ingested.[34] S. schenckii is also capable of modulating the immune response to promote its own survival by blocking cytokine production by macrophages.[34]
Specific
The specific immune response is active later in infection and involves both B cells and T cells. Severe sporotrichosis is rare in endemic areas where humans are in near constant contact with S. schenckii spores. This fact, combined with the increased severity of disease in immunocompromised patients points to an important role for specific immunity in S. schenckii infection.[34] Patients with sporotrichosis have been shown to produce antibodies specific to S. schenckii[36] and these antibodies may actually be protective against the disease.[2]
References
- 1 2 3 4 Vásquez-del-Mercado E, Arenas R, Padilla-Desgarenes C (July 2012). "Sporotrichosis". Clin. Dermatol. 30 (4): 437–43. doi:10.1016/j.clindermatol.2011.09.017. PMID 22682194.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 Barros MB, de Almeida Paes R, Schubach AO (October 2011). "Sporothrix schenckii and Sporotrichosis". Clin. Microbiol. Rev. 24 (4): 633–54. doi:10.1128/cmr.00007-11. PMC 3194828
 . PMID 21976602.
. PMID 21976602. - ↑ Rodriguez-Caban J, Gonzalez-Velazquez W, Perez-Sanchez L, Gonzalez-Mendez R, Rodriguez-del Valle N (2011). "Calcium/calmodulin kinase1 and its relation to thermotolerance and HSP90 in Sporothrix schenckii: an RNAi and yeast two-hybrid study". BMC Microbiol. 11: 162. doi:10.1186/1471-2180-11-162. PMC 3146815
 . PMID 21745372.
. PMID 21745372. - ↑ Toledo MS, Tagliari L, Suzuki E, Silva CM, Straus AH, Takahashi HK (2010). "Effect of anti-glycosphingolipid monoclonal antibodies in pathogenic fungal growth and differentiation. Characterization of monoclonal antibody MEST-3 directed to Manpalpha1-->3Manpalpha1-->2IPC". BMC Microbiol. 10: 47. doi:10.1186/1471-2180-10-47. PMC 2831884
 . PMID 20156351.
. PMID 20156351. - 1 2 3 Morris-Jones R, Youngchim S, Gomez BL, et al. (July 2003). "Synthesis of melanin-like pigments by Sporothrix schenckii in vitro and during mammalian infection". Infect. Immun. 71 (7): 4026–33. doi:10.1128/iai.71.7.4026-4033.2003. PMC 161969
 . PMID 12819091.
. PMID 12819091. - ↑ Mycology Online - University of Adelaide
- ↑ Pappas PG, Tellez I, Deep AE, Nolasco D, Holgado W, Bustamante B (January 2000). "Sporotrichosis in Peru: description of an area of hyperendemicity". Clin. Infect. Dis. 30 (1): 65–70. doi:10.1086/313607. PMID 10619735.
- ↑ Marimon R, Gené J, Cano J, Trilles L, Dos Santos Lazéra M, Guarro J (September 2006). "Molecular phylogeny of Sporothrix schenckii". J. Clin. Microbiol. 44 (9): 3251–6. doi:10.1128/jcm.00081-06. PMC 1594699
 . PMID 16954256.
. PMID 16954256. - 1 2 Dixon DM, Salkin IF, Duncan RA, et al. (June 1991). "Isolation and characterization of Sporothrix schenckii from clinical and environmental sources associated with the largest U.S. epidemic of sporotrichosis". J. Clin. Microbiol. 29 (6): 1106–13. PMC 269953
 . PMID 1864926.
. PMID 1864926. - ↑ "Sporotrichosis associated with Wisconsin sphagnum moss". MMWR Morb. Mortal. Wkly. Rep. 31 (40): 542–4. October 1982. PMID 6817054.
- ↑ "Multistate outbreak of sporotrichosis in seedling handlers, 1988". MMWR Morb. Mortal. Wkly. Rep. 37 (42): 652–3. October 1988. PMID 2971870.
- ↑ Barros MB, Schubach Ade O, do Valle AC, et al. (February 2004). "Cat-transmitted sporotrichosis epidemic in Rio de Janeiro, Brazil: description of a series of cases". Clin. Infect. Dis. 38 (4): 529–35. doi:10.1086/381200. PMID 14765346.
- 1 2 3 4 5 6 Kauffman CA, Bustamante B, Chapman SW, Pappas PG (November 2007). "Clinical practice guidelines for the management of sporotrichosis: 2007 update by the Infectious Diseases Society of America". Clin. Infect. Dis. 45 (10): 1255–65. doi:10.1086/522765. PMID 17968818.
- 1 2 al-Tawfiq JA, Wools KK (June 1998). "Disseminated sporotrichosis and Sporothrix schenckii fungemia as the initial presentation of human immunodeficiency virus infection". Clin. Infect. Dis. 26 (6): 1403–6. doi:10.1086/516356. PMID 9636870.
- ↑ Galhardo MC, Silva MT, Lima MA, et al. (June 2010). "Sporothrix schenckii meningitis in AIDS during immune reconstitution syndrome". J. Neurol. Neurosurg. Psychiatr. 81 (6): 696–9. doi:10.1136/jnnp.2009.173187. PMID 20392979.
- 1 2 3 4 5
- ↑ American Rose Society
- 1 2 3 4 Medscape
- ↑ American Veterinary Medical Association
- 1 2 3 Sporothrix spp. Doctor Fungus
- ↑ Ben-Ami R, Lewis RE, Raad II, Kontoyiannis DP (April 2009). "Phaeohyphomycosis in a tertiary care cancer center". Clin. Infect. Dis. 48 (8): 1033–41. doi:10.1086/597400. PMID 19267655.
- ↑ Singh MF, Fernandes SR, Samara AM (February 2004). "Sporothrix schenckii infection mimicking sarcoidosis". Rheumatology (Oxford). 43 (2): 248–9. doi:10.1093/rheumatology/keh010. PMID 14739470.
- ↑ Ishizaki H, Nakamura Y, Kariya H, Iwatsu T, Wheat R (1976). "Delayed hypersensitivity cross-reactions between Sporothrix schenckii and Ceratocystis species in sporotrichotic patients". J. Clin. Microbiol. 3 (6): 545–7. PMC 274353
 . PMID 59734.
. PMID 59734. - ↑ Fungal Molecular Diagnostics
- ↑ Hu S, Chung WH, Hung SI, et al. (April 2003). "Detection of Sporothrix schenckii in clinical samples by a nested PCR assay". J. Clin. Microbiol. 41 (4): 1414–8. doi:10.1128/jcm.41.4.1414-1418.2003. PMC 153868
 . PMID 12682123.
. PMID 12682123. - ↑ Almeida-Paes R, Pimenta MA, Pizzini CV, et al. (March 2007). "Use of mycelial-phase Sporothrix schenckii exoantigens in an enzyme-linked immunosorbent assay for diagnosis of sporotrichosis by antibody detection". Clin. Vaccine Immunol. 14 (3): 244–9. doi:10.1128/cvi.00430-06. PMC 1828849
 . PMID 17215334.
. PMID 17215334. - ↑ Trilles L, Fernández-Torres B, Dos Santos Lazéra M, et al. (September 2005). "In vitro antifungal susceptibilities of Sporothrix schenckii in two growth phases". Antimicrob. Agents Chemother. 49 (9): 3952–4. doi:10.1128/aac.49.9.3952-3954.2005. PMC 1195444
 . PMID 16127080.
. PMID 16127080. - 1 2 Sterling JB, Heymann WR (October 2000). "Potassium iodide in dermatology: a 19th century drug for the 21st century-uses, pharmacology, adverse effects, and contraindications". J. Am. Acad. Dermatol. 43 (4): 691–7. doi:10.1067/mjd.2000.107247. PMID 11004629.
- ↑ Revankar SG, Sutton DA (October 2010). "Melanized fungi in human disease". Clin. Microbiol. Rev. 23 (4): 884–928. doi:10.1128/cmr.00019-10. PMC 2952981
 . PMID 20930077.
. PMID 20930077. - ↑ Romero-Martinez R, Wheeler M, Guerrero-Plata A, Rico G, Torres-Guerrero H (June 2000). "Biosynthesis and functions of melanin in Sporothrix schenckii". Infect. Immun. 68 (6): 3696–703. doi:10.1128/iai.68.6.3696-3703.2000. PMC 97661
 . PMID 10816530.
. PMID 10816530. - ↑ Lima OC, Bouchara JP, Renier G, Marot-Leblond A, Chabasse D, Lopes-Bezerra LM (September 2004). "Immunofluorescence and flow cytometry analysis of fibronectin and laminin binding to Sporothrix schenckii yeast cells and conidia". Microb. Pathog. 37 (3): 131–40. doi:10.1016/j.micpath.2004.06.005. PMID 15351036.
- 1 2 3 4 Hogan LH, Klein BS, Levitz SM (October 1996). "Virulence factors of medically important fungi". Clin. Microbiol. Rev. 9 (4): 469–88. PMC 172905
 . PMID 8894347.
. PMID 8894347. - ↑ Tsuboi R, Sanada T, Ogawa H (July 1988). "Influence of culture medium pH and proteinase inhibitors on extracellular proteinase activity and cell growth of Sporothrix schenckii". J. Clin. Microbiol. 26 (7): 1431–3. PMC 266631
 . PMID 3045155.
. PMID 3045155. - 1 2 3 4 5 6 Carlos IZ, Sassá MF, da Graça Sgarbi DB, Placeres MC, Maia DC (July 2009). "Current research on the immune response to experimental sporotrichosis". Mycopathologia. 168 (1): 1–10. doi:10.1007/s11046-009-9190-z. PMID 19241140.
- ↑ Oda LM, Kubelka CF, Alviano CS, Travassos LR (February 1983). "Ingestion of yeast forms of Sporothrix schenckii by mouse peritoneal macrophages". Infect. Immun. 39 (2): 497–504. PMC 347978
 . PMID 6832808.
. PMID 6832808. - ↑ Scott EN, Muchmore HG (February 1989). "Immunoblot analysis of antibody responses to Sporothrix schenckii". J. Clin. Microbiol. 27 (2): 300–4. PMC 267296
 . PMID 2915023.
. PMID 2915023.
Further reading
- Fungus Page: Sporothrix schenckii, cause of Rose-picker's Disease
- EMedicine: Sporotrichosis
- Adelaide University: Sporothrix schenckii
- American Society for Microbiology: Sporothrix schenckii and Sporotrichosis
- Microbe wiki: Sporothrix schenckii