Senile plaques
Senile plaques (also known as neuritic plaques) are extracellular deposits of amyloid beta in the grey matter of the brain.[1][2] Degenerative neural structures and an abundance of microglia and astrocytes can be associated with senile plaque deposits. These deposits can also be a byproduct of senescence (ageing). However, large numbers of senile plaques and neurofibrillary tangles are characteristic features of Alzheimer's disease. Abnormal neurites in senile plaques are composed primarily of paired helical filaments, a component of neurofibrillary tangles.[3] The plaques are variable in shape and size, but are on average 50 µm in size.[4] In Alzheimer's disease they are primarily composed of amyloid beta peptides. These polypeptides tend to aggregate and are believed to be neurotoxic.
History
In 1892 Paul Blocq and Gheorghe Marinescu first described the presence of plaque deposits in grey matter.[5][6] As a result of their similarity to actinomyces druses, they were called druse necrosis by Oskar Fischer during the early 20th century. The connection between plaques and dementia was discovered by Alois Alzheimer in 1906.[7] By 1911 Max Bielschowsky proposed the amyloid-nature of plaque deposits. The same year Teofil Simchowicz introduced the term senile plaques.[8] Wisniewski coined the term neuritic plaques in 1973. The second half of the 20th century saw proposed theories of immunological and genetic factors in plaque formation.[9] Statistical investigations were performed by J.A.N. Corsellis and M. Franke in the 1970s. M. Franke showed that a demential disease is likely to occur when the number of senile plaques in the frontal cortex is more than 200/mm3. By 1985 beta amyloid formations were successfully identified through biochemical techniques, though many unsolved questions about the importance and formation of senile plaques remained.
Formation and description
Concentrated in the synapse of neurons is an amyloid precursor protein (APP) that extends across the plasma membrane. A portion of this protein contains an Aβ peptide sequence. This region comprises part of the DNA segment spanning APP that codes for proteins.[10]
In the formation of senile plaques, Aβ is cleaved from the amyloid precursor protein. Although three enzymes can process APP, only β-(beta) and γ-(gamma) secretase are directly involved in the formation of senile plaques. β-secretase (BACE) is a protease enzyme that cleaves proteins and peptides. This protease cleaves APP to further expose the carboxyl terminal fragments of Aβ. After the bulk of APP is released by this process, γ-secretase cleaves the remaining carboxyl fragments on the transmembrane domain. The sequential actions of γ-secretase following BACE activity results in Aβ protein fragments (amyloid beta) that are released into the extracellular space.[10] Eventually, the accumulation of amyloid beta outside of neuronal synapses forms an aggregate mass of plaque that pushes aside fine ramifications and connections of brain cells.
The formation of amyloid beta fragments is a normal occurrence in the human body. However, the accumulation of Aβ leading to the formation of plaque deposits is an unusual phenomenon. Although the cause of this abnormality is largely unknown, research has revealed certain species of amyloid beta that differ by a few amino acids in length that readily aggregate into plaques. These species are more pathogenic.[11]
In an article written by Stone J. it was proposed that the formation of senile plaques is initiated by the bleeding from a cerebral capillary, which creates the conditions for the formation of an amyloid-rich plaque. This suggests that the spread of plaque formation is the capillary bed of the cerebral cortex, which sheds light on why plaque formation is age-related, since with age the capillary bed becomes fragile. Stone also suggested that a hemorrhage can create the condition for the formation of plaques, this explained why the features of the plaques consisted of being small and uniform in size; each plaque being the site of a capillary bleed.[12]
Identification
_presenile_onset.jpg)
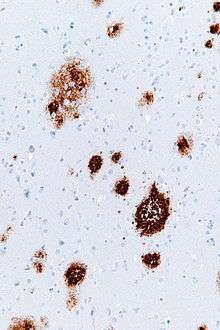
Senile plaques are visible in light microscopy using the staining techniques of silver, Congo red, Thioflavin, cresyl violet, and PAS-reaction. Plaque deposits are also visible through fluorescence and immunofluorescence microscopy.[3][13] Bielschowsky silver staining was found to be the least efficient means of visualizing senile plaques whereas Campbell and Gallyas silver staining techniques showed improved identification and accuracy. Using Congo red, only one-fourth of senile plaques present were noticeably stained.[11] Senile plaques may also be visualized with an immunostain directed against beta amyloid. The primary problem with the above staining methods is that sections of the neural tissue must be excised from the brain in order to accurately identify senile plaques. This is problematic because removing neural tissue can be as detrimental as the actual plaques themselves.
Disease
An important criterion of the neuropathological-histological verification of Alzheimer’s disease is the formation of senile plaques. Beta amyloid peptides associated with senile plaques have been found to play a central role in the risk, onset, and progression of Alzheimer's disease as well. Of particular importance is the longer species of beta amyloid known as beta amyloid 42. Elevated levels of beta amyloid, as well as an elevation in the ratio of beta amyloid 42 to the shorter major species of beta amyloid 40, has been identified as important in early events in the pathogenesis of Alzheimer's Disease.[14]
Other factors in Alzheimer's disease verification include pathological neurofibrillaries, tangles, and atrophic brain with hydrocephalus. The formation and the distribution of the pathological neurofibrillaries have a regularity[15] and allows one to determine the stage of the disease. In combination with the occurrence of a great number of plaques, Alzheimer’s disease can be diagnosed with high probability. A correlation between the presence of senile plaques and Down syndrome has also been verified.[1]
Occurrence
Senile plaques can be found in human and animal brains (e.g. mammals and birds). From an age of 60 years (10%) to an age of 80 years (60%), the proportion of people with senile plaques increases linearly. A small proportion of plaques that form can be due to the physiological process of aging. Women are slightly more likely to have plaques than men.[4] The plaques occur commonly in the amygdaloid nucleus and the sulci of the cortex of brain.
Research
An increasing variety of compounds that reduce beta amyloid levels are being identified. Several of these compounds have beta amyloid 42 selectivity whereas others attempt to modulate amyloid precursor protein. Such compounds are now reaching clinical evaluation to determine how they may be of benefit in the treatment of Alzheimer's disease.[14]
See also
References
- 1 2 Cras P; Kawai M; Lowery D; Gonzalez-DeWhitt P; Greenberg B; Perry G (September 1991). "Senile plaque neurites in Alzheimer disease accumulate amyloid precursor protein". Proceedings of the National Academy of Sciences of the United States of America. 88 (17): 7552–6. doi:10.1073/pnas.88.17.7552. PMC 52339
 . PMID 1652752.
. PMID 1652752. - ↑ Purves, Dale; Augustine, George J.; Fitzpatrick, David; Hall, William C.; LaManita, Anthony-Samuel; White, Leonard E.; Mooney, Richard D.; Platt, Michael L. (2012). Neuroscience (5th ed.). Sunderland, MA: Sinauer Associates. p. 713. ISBN 978-0-87893-695-3.
- 1 2 Ksiezak-Reding H, Morgan K, Mattiace LA, et al. (December 1994). "Ultrastructure and biochemical composition of paired helical filaments in corticobasal degeneration". The American Journal of Pathology. 145 (6): 1496–508. PMC 1887493
 . PMID 7992852.
. PMID 7992852. - 1 2 Franke, M (1976). "Statistische Untersuchungen über die senilen Drusen im menschlichen Gehirn / Thesen". Berlin, Germany: Neuropathologische Abteilung.
- ↑ Blocq, Paul; Marinesco, Georges (1892). Sur les lesions et la pathogenie de l’epilepsie dite essentielle. pp. 445–6. OCLC 492619936.
- ↑ Buda O; Arsene D; Ceausu M; Dermengiu D; Curca GC (January 2009). "Georges Marinesco and the early research in neuropathology". Neurology. 72 (1): 88–91. doi:10.1212/01.wnl.0000338626.93425.74. PMID 19122036.
- ↑ Alzheimer, A (1907). "Uber einen eigenartige Erkranung der Hirnrinde". Allgemeine Zeitschrift für Psychiatrie und Psychisch-Gerichtlich Medizin. 64: 146–8.
- ↑ Simchowicz T.: Histologische Studien über die senile Demenz. in: Nissl F., Alzheimer A. (Hrsg.): Histologische und histopathologische Arbeiten über die Grosshirnrinde mit besonderer Berücksichtigung der pathologischen Anatomie der Geisteskrankheiten. Jena: G. Fischer, 1911, p. 267–444.
- ↑ Op den Velde W; Stam FC (January 1976). "Some cerebral proteins and enzyme systems in Alzheimer's presenile and senile dementia". Journal of the American Geriatrics Society. 24 (1): 12–6. PMID 1244383.
- 1 2 Suh YH; Checler F (September 2002). "Amyloid precursor protein, presenilins, and alpha-synuclein: molecular pathogenesis and pharmacological applications in Alzheimer's disease". Pharmacological Reviews. 54 (3): 469–525. doi:10.1124/pr.54.3.469. PMID 12223532.
- 1 2 Mavrogiorgou P; Gertz HJ; Ferszt R; Wolf R; Bär KJ; Juckel G (December 2011). "Are routine methods good enough to stain senile plaques and neurofibrillary tangles in different brain regions of demented patients?" (PDF). Psychiatria Danubina. 23 (4): 334–9. PMID 22075733.
- ↑ Stone J (September 2008). "What initiates the formation of senile plaques? The origin of Alzheimer-like dementias in capillary haemorrhages". Medical Hypotheses. 71 (3): 347–59. doi:10.1016/j.mehy.2008.04.007. PMID 18524497.
- ↑ Lamy C, Duyckaerts C, Delaere P, et al. (1989). "Comparison of seven staining methods for senile plaques and neurofibrillary tangles in a prospective series of 15 elderly patients". Neuropathology and Applied Neurobiology. 15 (6): 563–78. doi:10.1111/j.1365-2990.1989.tb01255.x. PMID 2482455.
- 1 2 Findeis MA (November 2007). "The role of amyloid beta peptide 42 in Alzheimer's disease". Pharmacology & Therapeutics. 116 (2): 266–86. doi:10.1016/j.pharmthera.2007.06.006. PMID 17716740.
- ↑ Braak H; Braak E; Bohl J (1993). "Staging of Alzheimer-related cortical destruction". European Neurology. 33 (6): 403–8. doi:10.1159/000116984. PMID 8307060.
Further reading
- Jellinger KA. Neurodegenerative Erkrankungen (ZNS) - Eine aktuelle Übersicht. Journal für Neurologie, Neurochirurgie und Psychiatrie. 2005;6(1):9-18.
- Cruz L, Urbanc B, Buldyrev SV, et al. (July 1997). "Aggregation and disaggregation of senile plaques in Alzheimer disease". Proceedings of the National Academy of Sciences of the United States of America. 94 (14): 7612–6. doi:10.1073/pnas.94.14.7612. PMC 23870
 . PMID 9207140.
. PMID 9207140. - Stone J (September 2008). "What initiates the formation of senile plaques? The origin of Alzheimer-like dementias in capillary haemorrhages". Medical Hypotheses. 71 (3): 347–59. doi:10.1016/j.mehy.2008.04.007. PMID 18524497.