Romano–Ward syndrome
| Romano–Ward syndrome | |
|---|---|
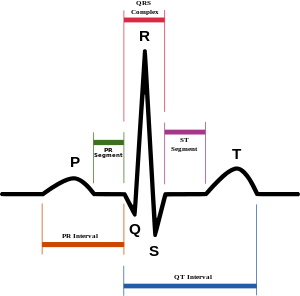 | |
| Schematic representation of normal ECG trace (sinus rhythm), with waves, segments, and intervals labeled. | |
| Classification and external resources | |
| ICD-9-CM | 794.31 |
| OMIM | 192500 |
| DiseasesDB | 11661 |
| MeSH | D029597 |
Romano–Ward syndrome is the major variant of long QT syndrome. It is a condition that causes a disruption of the heart's normal rhythm. This disorder is a form of long QT syndrome, which is a heart condition that causes the cardiac muscle to take longer than usual to recharge between beats. If untreated, the irregular heartbeats can lead to fainting, seizures, or sudden death.
Inheritance

Romano–Ward syndrome is inherited in an autosomal dominant pattern. It is the most common form of inherited long QT syndrome, affecting an estimated 1 in 5,000 people worldwide, although more people may be affected but never experience any signs or symptoms of the condition.
Causes
Mutations in the ANK2, KCNE1, KCNE2, KCNH2, KCNQ1, and SCN5A genes can cause Romano–Ward syndrome. The proteins made by most of these genes form channels that transport positively-charged ions, such as potassium and sodium, in and out of cells. In cardiac muscle, these ion channels play critical roles in maintaining the heart's normal rhythm. Mutations in any of these genes alter the structure or function of channels, which changes the flow of ions between cells. A disruption in ion transport alters the way the heart beats, leading to the abnormal heart rhythm characteristic of Romano–Ward syndrome.
Unlike most genes related to Romano–Ward syndrome, the ANK2 gene does not produce an ion channel. The protein made by the ANK2 gene ensures that other proteins, particularly ion channels, are inserted into the cell membrane appropriately. A mutation in the ANK2 gene likely alters the flow of ions between cells in the heart, which disrupts the heart's normal rhythm and results in the features of Romano–Ward syndrome.
This article incorporates public domain text from The U.S. National Library of Medicine
Treatment
An imbalance between the right and left sides of the sympathetic nervous system may play a role in the etiology of this syndrome. The imbalance can be temporarily abolished with a left stellate ganglion block, which shorten the QT interval. If this is successful, surgical ganglionectomy can be performed as a permanent treatment.[1]
References
- ↑ Hines, Roberta, Soeltin's Anesthesia and Co-existing Disease (4 ed.), Elsevir, p. 89