Rheumatoid nodule
| Rheumatoid nodule | |
|---|---|
 | |
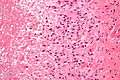
| Micrograph of a rheumatoid nodule, showing the characteristic palisading granuloma with a core consisting of necrotic collagen and fibrin. H&E stain. | |
| Classification and external resources | |
| ICD-10 | M06.3 |
| MeSH | D012218 |
A rheumatoid nodule is a local swelling or tissue lump, usually rather firm to touch, like an unripe fruit, which occurs almost exclusively in association with rheumatoid arthritis. Very rarely rheumatoid nodules occur as rheumatoid nodulosis in the absence of arthritis. They are usually subcutaneous especially over bony prominences such as the olecranon (tip of the elbow) or the interphalangeal joints (finger knuckles). Less commonly they occur in the lining of the lung and other internal organs. The occurrence of nodules in the lung of miners exposed to silica dust was known as Caplan's syndrome. Nodules vary in size from that of a lentil or pea to that of a mandarin orange. Quite often they are associated with synovial pockets or bursae. About 5% of rheumatoid arthritis patients have such nodules within two years of disease onset, and the cumulative prevalence is about 25%. In the great majority of cases nodules are not painful or disabling in any way, being more of an unsightly nuisance, but in some cases they can be painful, especially if the overlying skin breaks down.[1] Rarely, the nodules occur at diverse sites on body (e.g. upper eyelid, distal region of the soles of the feet, vulva and internally in the gallbladder, lung, heart valves, larynx, and spine).[2]
Pathology
Histological examination of nodules shows that they consist of a shell of fibrous tissue surrounding a center of fibrinoid necrosis. Pea-sized nodules have one centre. Larger nodules tend to be multilocular, with many separate shells or with connections between the necrotic centres. Individual necrotic centres may contain a cleft or several centres of necrosis may all open on to a large bursal pocket containing synovial fluid.
The boundary between the necrotic centre and the outer fibrous shell is made up of the characteristic feature of the nodule, which is known as a cellular palisade. The palisade is a densely packed layer of macrophages and fibroblasts which tend to be arranged radially, like the seeds of a kiwifruit or fig. Further out into the fibrous shell there is a zone that contains T cells and plasma cells in association with blood vessels.
The overall histological picture is essentially identical to that of rheumatoid synovitis with the main differences being that the palisade replaces the synovial intima (they may blend imperceptibly in bursae) and an almost total absence of B cells.
Histopathology images
Treatment
Treatment of rheumatoid nodules is rarely a priority for people with rheumatoid arthritis. However, surgical removal is often successful, even if there is a tendency for nodules to regrow. Of the drug therapies commonly used in rheumatoid arthritis, methotrexate has the disadvantage of tending to make nodules worse. TNF inhibitors do not have a very reliable effect on nodules. B cell depletion with rituximab often leads to disappearance of nodules but this is not guaranteed.
References
- ↑ Carmona L, González-Alvaro I, Balsa A, Angel Belmonte M, Tena X, Sanmartí R (September 2003). "Rheumatoid arthritis in Spain: occurrence of extra-articular manifestations and estimates of disease severity". Ann. Rheum. Dis. 62 (9): 897–900. doi:10.1136/ard.62.9.897. PMC 1754657
 . PMID 12922967..
. PMID 12922967.. - ↑ Upile T, Jerjes W, Sipaul F, Singh S, Hopper C, Wright A, Sandison A (2007). "Rheumatoid nodule of the thyrohyoid membrane: a case report". J Med Case Rep. 1: 123. doi:10.1186/1752-1947-1-123. PMC 2174496
 . PMID 17974016.
. PMID 17974016.



.jpg)