Primidone
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Lepsiral, Mysoline, Resimatil, Primaclone |
| AHFS/Drugs.com | Monograph |
| Pregnancy category |
|
| Dependence liability | Moderate-high |
| Routes of administration | Oral |
| ATC code | N03AA03 (WHO) |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | ~100%[1] |
| Protein binding | 25%[1] |
| Metabolism | Hepatic |
| Biological half-life |
Primidone: 5-18 h, Phenobarbital: 75-120 h,[1] PEMA: 16 h[2] Time to reach steady state: Primidone: 2-3 days, Phenobarbital&PEMA 1-4weeks[3] |
| Excretion | Renal |
| Identifiers | |
| |
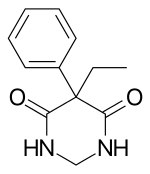
| Synonyms | desoxyphenobarbital, desoxyphenobarbitone |
| CAS Number |
125-33-7 |
| PubChem (CID) | 4909 |
| DrugBank |
DB00794 |
| ChemSpider |
4740 |
| UNII |
13AFD7670Q |
| KEGG |
D00474 |
| ChEBI |
CHEBI:8412 |
| ChEMBL |
CHEMBL856 |
| ECHA InfoCard | 100.004.307 |
| Chemical and physical data | |
| Formula | C12H14N2O2 |
| Molar mass | 218.252 g/mol |
| 3D model (Jmol) | Interactive image |
| |
| |
| | |
Primidone (INN, BAN, USP) is an anticonvulsant of the barbiturate class. It is a structural analog of phenobarbital and related to barbiturate-derivative anticonvulsants. The active metabolites, phenobarbital, p-hydroxyphenobarbital, and phenylethylmalonamide, are also anticonvulsants. Primidone was once a mainstay anticonvulsant in the treatment of partial and generalized seizures and was the treatment of choice for secondarily generalized seizures originating in the temporal lobes, especially when combined with phenytoin, but by the early 1980s, carbamazepine had surpassed it in popularity due to the latter's lower incidence of sedation. As time passed and more and more anticonvulsants came on the market, primidone was pushed further and further away from its former place of prominence, and major Western pharmaceutical corporations became less and less interested in manufacturing and selling it. It has largely fallen into disuse in the developed world as more and more anticonvulsants entered the market, and it has been withdrawn from various markets around the world.
Medical uses
Epilepsy
Licensed for generalized tonic-clonic and complex partial seizures in the United Kingdom.[4] In the United States, primidone is approved for adjunctive (in combination with other drugs) and monotherapy (by itself) use in generalized tonic-clonic seizures, simple partial seizures, and complex partimple partial seizures, and myoclonic seizures.[4] In juvenile myoclonic epilepsy (JME), it is a second-line therapy, reserved for when the valproates and/or lamotrigine do not work and when other second-line therapies—acetazolamid work either.[5]
Open-label case series have suggested that primidone is effective in the treatment of epilepsy.[6][7][8][9][10][11] Primidone has been compared to carbamazepine,[12][13][14][15] phenytoin,[13][14][16][17] phenobarbital,[13][14][16] mephobarbital, ethotoin, metharbital, and mephenytoin.[16] Compared to carbamazepine, primidone has been found to be equally effective,[12] less effective at controlling partial seizures but just as effective at controlling generalized tonic-clonics,[13][15] less likely to cause side effects but more likely to cause side effects requiring withdrawal of the drug, half as likely to reduce seizures in patients being considered for surgery by at least 80%,[14] more likely to cause depression,[12] significantly more likely cause intolerable side effects,[15] more likely to cause impotence and decreased libido,[13] and cause more adverse effects on motor performance and attention/concentration tests.[12][15] In adult comparison trials, primidone had a higher incidence of intolerable side effects than phenytoin,[15] a higher incidence of decreased libido and impotence, similar control of tonic-clonic seizures, more likely to cause nausea, vomiting, dizziness, and sedation;[13] twice as likely to be effective in controlling seizures in epilepsy surgery candidates,[14] more acute effects such as nausea, vomiting, dizziness, and sedation,[13] and to be just as effective.[16][17]
Essential tremor
Primidone is considered to be a first-line therapy for essential tremor along with propranolol. In terms of tremor amplitude reduction, it is just as effective as propranolol, reducing it by 50%. Both drugs are well studied for this condition, unlike other therapies, and are recommended for initial treatment. 25 mg/day (low-dose therapy) is just as good as 75 mg/day (high-dose therapy).[18]
Primidone is not the only anticonvulsant used for essential tremor; the others include topiramate (Topamax) and gabapentin (Neurontin). Other pharmacological agents include alprazolam (Xanax), clonazepam (Klonopin), atenolol, sotalol, nadolol, clozapine, nimodipine, and botilinum toxin A. Many of these drugs were less effective (according to Table 1), but a few were not. Only propranolol has been compared to primidone in a clinical trial.[18]
Long QT syndrome
The first case report in which the shortening of the QT interval by primidone was documented, published in the July 1980 issue of Annals of Internal Medicine, involved three patients, a 31-year-old woman, her 15-year-old nephew, and his 16-year-old sister. The woman still had ventricular fibrillation, syncope, and seizures even after the removal of her left stellate ganglion and a thoracic chain dissection. The woman had previously been tried on a combination of phenobarbital and phenytoin when she was thought to have only seizures, followed by phenobarbital combined phenytoin and procainamide. The procainamide was replaced with propanolol, which in turn replaced the propanolol when the latter brought the tachycardia back almost instantaneously upon the first dose. The phenobarbital and phenytoin were then combined with atropine and acetyl strophanthidin. When this failed, the atropine and acetyl strophanthidin were replaced with lidocaine prior to the surgery. After the surgery, the QT-prolongation returned, so the phenytoin was doubled to 200 mg four times daily. A month later, she was admitted to the hospital for phenytoin toxicity, where it was found that she had slow spike and abortive wave activity in her left temporal lobe. It was after this that primidone was substituted for phenytoin. The primidone suppressed the fibrillations and lengthened the QT interval for two years and eight months in the patient. Her 16-year-old niece was started on primidone after an unsuccessful trial of phenytoin. Following this, her 15-year-old nephew, the niece's brother, was started because of family history.[19]
The second case report, published in the December 1986 issue of Zhonghua Xin Xue Guan Bing Za Zhi, describes four cases, men, women, adults and adolescents, who were put on primidone for LQTS.[20] The 2002 case focuses on hypocalcemia stemming from such treatment in an adolescent male. The primidone he had been taking suppressed his hypocalcemia-induced QT prolongation.[21]
Psychiatric disorders
In 1965, Monroe and Wise reported using primidone along with a phenothiazine derivative antipsychotic and chlordiazepoxide in treatment-resistant psychosis.[22] What is known is that ten years later, Monroe went on to publish the results of a meta-analysis of two controlled clinical trials on people displaying out-of-character and situationally inappropriate aggression, who had abnormal EEG readings, and who responded poorly to antipsychotics; one of the studies was specifically mentioned as involving psychosis patients. When they were given various anticonvulsants not only did their EEGs improve, but so did the aggression.[23]
In March 1993, S.G. Hayes of the University of Southern California School of Medicine reported that nine out of twenty-seven people (33%) with either treatment-resistant depression or treatment-resistant bipolar disorder had a permanent positive response to primidone. It should be noted that a plurality of subjects were also given methylphenobarbital in addition to or instead of primidone.[24]
Five months later, Brown, Stone, and Rathbone published a case report titled, "Primidone and rapid cycling affective disorders" describing a 62-year-old woman who had rapid-cycling bipolar disorder starting in 1978. Lithium treatment was started two years later, but it only eliminated the manic swings, leaving her depressions unaffected. Between 1980 and 1989, the patient had six to ten episodes a year, each lasting between eleven and twenty-four days that left her with little energy, made tasks seem more arduous than they actually were, a smaller appetite, a tendency to sleep too much, anxious, and weepy. No antidepressant eliminated all her symptoms. At the age of fifty-eight, she was started on 125 mg/day of primidone for hand tremor. Her depression, which was resistant to all the antidepressants she tried, gradually remitted during primidone therapy; the expected depressive episode lasted three days instead of 13-17. Eight weeks later, she had an episode lasting twenty-eight days. Her last two episodes were nineteen weeks apart, lasting twenty-five and twenty-seven days, respectively. It was during the final episode, in the middle of 1990, that her dose of primidone was stabilized at 500 mg/day. She had been free of depression for two and a half years before the case report was written up.[25]
In 1999, Drs. Linda C. Schaffer, Charles B. Schaffer, and J. Caretto conducted a follow-up study on those earlier reports, as no one else had done so in the six years following their publication, and found it to be roughly as (permanently) effective for refractory bipolar disorder as Hayes had reported it to be (31% vs. Hayes's 33%). All subjects with a permanent and complete treatment response were either Bipolar I or Bipolar NOS. In this study, unlike the 1993 case report, primidone affected manic symptoms—especially insomnia, anxiety, and racing thoughts—and only on manic symptoms.[26]
Other
Unlike carbamazepine, there are few case reports mentioning the use of primidone in the treatment of trigeminal neuralgia. The first, published in the October 10, 1957 issue of Gazette Médicale de France, has no abstract.[27] The second one was a case report of a woman taking primidone and then phenobarbital for trigeminal neuralgia. She developed toxic epidermal necrolysis, as well as endocarditis and gastrointestinal hemorrhage. The second recurrence, induced by phenobarbital, killed her within five weeks of onset.[28]
Two trials of primidone for athetosis have been published. In one, small doses of primidone successfully treated eighteen out of thirty-one children. In a subsequent pilot trial in which children who experienced improvement were switched to placebo, the results were much more disappointing, with the two subjects who experienced subjective improvement also experiencing this on placebo.[29]
Primidone has been used in cerebral palsy. In 1953, Plum and Sparup found that out of thirty-three patients, twenty had a favorable or moderate response. Thorn reported in 1962 that sixteen patients responded favorably to both primidone and chlordiazepoxide and four to only primidone. Nine patients responded only to chlordiazepoxide and four responded to neither drug. The best results were obtained in athetosis and rigidity.[30]
Primidone has veterinary uses, including the prevention of aggressive behavior and cannibalism in gilt pigs, and treatment of nervous disorders in dogs and other animals.[31][32]
Adverse effects
Primidone can cause drowsiness, listlessness, ataxia, visual disturbances, nystagmus, headache, and dizziness. These side effects are the most common, occurring in more than 1% of users.[33] Transient nausea and vomiting are also common side effects.[13]

Dupuytren's contracture, a disease of the fasciae in the palm and fingers that permanently bends the fingers (usually the little and ring fingers) toward the palm, was first noted to be highly prevalent in epileptic people in 1941 by a Dr. Lund, fourteen years before primidone was on the market. Lund also noted that it was equally prevalent in individuals with idiopathic and symptomatic epilepsy and that the severity of the epilepsy did not matter. However, only one quarter of the women were affected vs. half of the men.[34] Thirty-five years later, Critcheley et al. reported a correlation between how long a patient had had epilepsy and his or her chance of getting Dupuytren's contracture. They suspected that this was due to phenobarbital therapy, and that the phenobarbital was stimulating peripheral tissue growth factors.[35] Dupuytren's contracture is almost exclusively found in Caucasians, especially those of Viking descent, and highest rates are reported in Northern Scotland, Norway, Iceland, and Australia. It has also been associated with alcoholism, heavy smoking, diabetes mellitus, physical trauma (either penetrating in nature or due to manual labor), tuberculosis, and HIV. People with rheumatoid arthritis are less likely to get this, and Drs. Hart and Hooper speculate that this is also true of gout due to the use of allopurinol This is the only susceptibility factor that is generally agreed upon. Anticonvulsants do not seem to increase the incidence of Dupuytren's contracture in non-whites.[34]
Primidone has other cardiovascular effects in beyond shortening the QT interval. Both it and phenobarbital are associated with elevated serum levels (both fasting and six hours after methionine loading) of homocysteine, an amino acid derived from methionine. This is almost certainly related to the low folate levels reported in primidone users. Elevated levels of homocysteine have been linked to coronary heart disease. In 1985, both drugs were also reported to increase serum levels of high density lipoprotein (HDL) cholesterol, total cholesterol, and apolipoproteins A and B.[36]
It was first reported to exacerbate hepatic porphyria in 1975. In 1981, it was shown that phenobarbital, one of primidone's metabolites, only induced a significant porphyrin at high concentrations in vitro.[37] It can also cause elevations in hepatic enzymes such as gamma-glutamyl transferase and alkaline phosphatase.[33]
Less than 1% of primidone users will experience a rash. Compared to carbamazepine, lamotrigine, and phenytoin, this is very low. The rate is comparable to that of felbamate, vigabatrin, and topiramate.[38] Primidone also causes exfoliative dermatitis, Stevens–Johnson syndrome, and toxic epidermal necrolysis.[33]

Primidone, along with phenytoin and phenobarbital, is one of the anticonvulsants most heavily associated with bone diseases such as osteoporosis, osteopenia (which can precede osteoporosis), osteomalacia and fractures.[39][40][41] The populations usually said to be most at risk are institutionalized people, postmenopausal women, older men, people taking more than one anticonvulsant, and children, who are also at risk of rickets.[39] However, it has been suggested that bone demineralization in most pronounced young people (25–44 years of age)[40] and one 1987 study of institutionalized people found that the rate of osteomalacia in the ones taking anticonvulsants—one out of nineteen individuals taking an anticonvulsant (vs. none among the thirty-seven people taking none) —was similar to that expected in elderly people. The authors speculated that this was due to improvements in diet, sun exposure and exercise in response to earlier findings, and/or that this was because it was sunnier in London than in the Northern European countries which had earlier reported this effect.[41] In any case, the use of more than one anticonvulsant has been associated with an increased prevalence of bone disease in institutionalized epilepsy patients versus institutionalized people who did not have epilepsy. Likewise, postmenopausal women taking anticonvulsants have a greater risk of fracture than their drug-naive counterparts.[39]
Anticonvulsants affect the bones in many ways. They cause hypophosphatemia, hypocalcemia, low Vitamin D levels, and increased parathyroid hormone. Anticonvulsants also contribute to the increased rate of fractures by causing somnolence, ataxia, and tremor which would cause gait disturbance, further increasing the risk of fractures on top of the increase due to seizures and the restrictions on activity placed on epileptic people.Increased fracture rate has also been reported for carbamazepine, valproate and clonazepam. The risk of fractures is higher for people taking enzyme-inducing anticonvulsants than for people taking non-enzyme-inducing anticonvulsants.[40] In addition to all of the above, primidone can cause arthralgia.[33]
Granulocytopenia, agranulocytosis, and red-cell hypoplasia and aplasia, and megaloblastic anemia are rarely associated with the use of primidone.[42] Megaloblastic anemia is actually a group of related disorders with different causes that share morphological characteristics—enlarged red blood cells with abnormally high nuclear-cytoplasmic ratios resulting from delayed maturation of nuclei combined with normal maturation of cytoplasm, into abnormal megakaryocytes and sometimes hypersegmented neutrophils; regardless of etiology, all of the megaloblastic anemias involve impaired DNA replication.[43] The anticonvulsant users who get this also tend to eat monotonous diets devoid of fruits and vegetables.[44]
This antagonistic effect is not due to the inhibition of dihydrofolate reductase, the enzyme responsible for the reduction of dihydrofolic acid to tetrahydrofolic acid, but rather to defective folate metabolism.[45]
In addition to increasing the risk of megaloblastic anemia, primidone, like other older anticonvulsants also increases the risk of neural tube defects,[46] and like other enzyme-inducing anticonvulsants, it increases the likelihood of cardiovascular defects, and cleft lip without cleft palate.[47] Epileptic women are generally advised to take folic acid,[46] but there is conflicting evidence regarding the effectiveness of vitamin supplementation in the prevention of such defects.[47][48]
Additionally, a coagulation defect resembling Vitamin K deficiency has been observed in newborns of mothers taking primidone.[46] Because of this, primidone is a Category D medication.[49]
Primidone, like phenobarbital and the benzodiazepines, can also cause sedation in the newborn and also withdrawal within the first few days of life; phenobarbital is the most likely out of all of them to do that.[46]
In May 2005, Dr. M. Lopez-Gomez's team reported an association between the use of primidone and depression in epilepsy patients; this same study reported that inadequate seizure control, posttraumatic epilepsy, and polytherapy were also risk factors. Polytherapy was also associated with poor seizure control. Out of all of the risk factors, usage of primidone and inadequate seizure control were the greatest; with ORs of 4.089 and 3.084, respectively. They had been looking for factors associated with depression in epilepsy patients.[50] Schaffer et al. 1999 reported that one of their treatment failures, a 45-year-old woman taking 50 mg a day along with lithium 600 mg/day, clozapine 12.5 mg/day, trazodone 50 mg/day, and alprazolam 4 mg/day for three and a half months experienced auditory hallucinations that led to discontinuation of primidone.[26] It can also cause hyperactivity in children;[51] this most commonly occurs at low serum levels.[52] There is one case of an individual developing catatonic schizophrenia when her serum concentration of primidone went above normal.[53]
Primidone is one of the anticonvulsants associated with anticonvulsant hypersensitivity syndrome, others being carbamazepine, phenytoin, and phenobarbital. This syndrome consists of fever, rash, peripheral leukocytosis, lymphadenopathy, and occasionally hepatic necrosis.[54]
Hyperammonemic encephalopathy was reported by Katano Hiroyuki of the Nagoya City Higashi General Hospital in early 2002 in a patient who had been stable on primidone monotherapy for five years before undergoing surgery for astrocytoma, a type of brain tumor. Additionally, her phenobarbital levels were inexplicably elevated post-surgery. This is much more common with the valproates than with any of the barbiturates.[55] A randomized controlled trial whose results were published in the July 1985 issue of The New England Journal of Medicine found that primidone was more likely to cause impotence than phenytoin, carbamazepine, or phenobarbital.[13] Like phenytoin, primidone is rarely associated with lymphadenopathy.[56] Primidone can also cause vomiting; this happens in 1.0–0.1% of users.[33]
Overdose
The most common symptoms of primidone overdose are coma with loss of deep tendon reflexes and, during the recovery period, if the patient survives, disorientation, dysarthria, nystagmus, and ataxia,[57] lethargy, somnolence, vomiting, nausea, and occasionally, focal neurological deficits which lessen over time.[58] Complete recovery comes within five to seven days of ingestion.[57] The symptoms of primidone poisoning have generally been attributed to its biotransformation to phenobarbital; however, primidone has toxic effects independent of its metabolites in humans.[58] The massive crystalluria that sometimes occurs sets its symptom profile apart from that of phenobarbital.[57][59][60][61] The crystals are white,[58][60] needle-like,[59] shimmering, hexagonal plates consisting mainly of primidone.[58][60]
In the Netherlands alone, there were thirty-four cases of suspected primidone poisoning between 1978 and 1982. Out of these, Primidone poisoning was much less common than phenobarbital poisoning. Twenty-seven of those adult cases were reported to the Dutch National Poison Control Center. Out of these, one person taking it with phenytoin and phenobarbital died, twelve became drowsy and four were comatose.[59]
Treatments for primidone overdose have included hemoperfusion with forced diuresis,[59] a combination of bemegride and amiphenazole;[62] and a combination of bemegride, spironolactone, caffeine, pentylenetetrazol, strophanthin, penicillin and streptomycin.[63]
In the three adults who are reported to have succumbed, the doses were 20–30 g.[57][62][63] However, two adult survivors ingested 30 g[57] 25 g,[62] and 22.5 g.[58] One woman experienced symptoms of primidone intoxication after ingesting 750 mg of her roommate's primidone.[64]
Interactions
Taking primidone with monoamine oxidase inhibitors (MAOIs) such as isocarboxazid (Marplan), phenelzine (Nardil), procarbazine (Matulane), selegiline (Eldepryl), tranylcypromine (Parnate) or within two weeks of stopping any one of them may potentiate the effects of primidone or change one's seizure patterns.[65] Isoniazid, an antitubercular agent with MAOI properties, has been known to strongly inhibit the metabolism of primidone.[66]
Like many anticonvulsants, primidone interacts with other anticonvulsants. Clobazam decreases clearance of primidone,[67] Mesuximide increases plasma levels of phenobarbital in primidone users,[68] both primidone and phenobarbital accelerate the metabolism of carbamazepine via CYP3A4,[69] and lamotrigine's apparent clearance is increased by primidone.[70] In addition to being an inducer of CYP3A4, it is also an inducer of CYP1A2, which causes it to interact with substrates such as fluvoxamine, clozapine, olanzapine, and tricyclic antidepressants.[71] It also interacts with CYP2B6 substrates such as bupropion, efavirenz, promethazine, selegiline, and sertraline; CYP2C8 substrates such as amiodarone, paclitaxel, pioglitazone, repaglinide, and rosiglitazone; and CYP2C9 substrates such as bosentan, celecoxib, dapsone, fluoxetine, glimepiride, glipizide, losartan, montelukast, nateglinide, paclitaxel, phenytoin, sulfonamides, trimethoprim, warfarin, and zafirlukast. It also interacts with estrogens.[65]
Primidone and the other enzyme-inducing anticonvulsants can cut the half-life of antipyrine roughly in half (6.2 ± 1.9 h vs. 11.2 ± 4.2 h), and increases the clearance rate by almost 70%. Phenobarbital reduces the half-life to 4.8 ± 1.3 and increases the clearance by almost 109%.[72] It also interferes with the metabolism of dexamethasone, a synthetic steroid hormone, to the point where its withdrawal from the regimen of a 14-year-old living in the United Kingdom made her hypercortisolemic.[73] Tempelhoff and colleagues at the Washington University School of Medicine's Department of Anesthesiology reported in 1990 that primidone and other anticonvulsant drugs increase the amount of fentanyl needed during craniotomy based on the patient's heart rate.[74]
Mechanism of action
The exact mechanism of primidone's anticonvulsant action is still unknown after over fifty years.[75] It is believed to work via interactions with voltage-gated sodium channels which inhibit high-frequency repetitive firing of action potentials.[76] The effect of primidone in essential tremor is not mediated by PEMA.[77] The major metabolite, phenobarbital, is also a potent anticonvulsant in its own right and likely contributes to primidone's effects in many forms of epilepsy. According to Brenner's Pharmacology textbook, Primidone also increases GABA-mediated chloride flux: thereby hyperpolarizing the membrane potential.
Pharmacokinetics
Primidone converts to phenobarbital and PEMA;[78] it is still unknown which exact cytochrome P450 enzymes are responsible.[66] The phenobarbital, in turn, is metabolized to p-hydroxyphenobarbital.[79] The rate of primidone metabolism was greatly accelerated by phenobarbital pretreatment, moderately accelerated by primidone pretreatment, and reduced by PEMA pretreatment.[80] In 1983, a new minor metabolite, p-hydroxyprimidone, was discovered.[81]
Primidone, carbamazepine, phenobarbital and phenytoin are among the most potent hepatic enzyme inducing drugs in existence. This enzyme induction occurs at therapeutic doses. In fact, people taking these drugs have displayed the highest degree of hepatic enzyme induction on record.[72] In addition to being an inducer of CYP3A4, it is also an inducer of CYP1A2, which causes it to interact with substrates such as fluvoxamine, clozapine, olanzapine, and tricyclic antidepressants, as well as potentially increasing the toxicity of tobacco products. Its metabolite, phenobarbital, is a substrate of CYP2C9,[71] CYP2B6,[82] CYP2C8, CYP2C19, CYP2A6, CYP3A5,[83] CYP1E1, and the CYP2E subfamily.[84] The gene expression of these isoenzymes is regulated by human pregnane receptor X (PXR) and constitutive androstane receptor (CAR). Phenobarbital induction of CYP2B6 is mediated by both.[83][85] Primidone does not activate PXR.[86]
The rate of metabolism of primidone into phenobarbital was inversely related to age; the highest rates were in the oldest patients (the maximum age being 55).[87] People aged 70–81, relative to people aged 18–26, have decreased renal clearance of primidone, phenobarbital, and PEMA, in ascending order of significance, and that there was a greater proportion of PEMA in the urine.[88] The clinical significance is unknown.
The percentage of primidone converted to phenobarbital has been estimated to be 5% in dogs and 15% in humans. Work done twelve years later found that the serum phenobarbital 0.111 mg/100 mL for every mg/kg of primidone ingested. Authors publishing a year earlier estimated that 24.5% of primidone was metabolized to phenobarbital. However, the patient reported by Kappy and Buckley would have had a serum level of 44.4 mg/100 mL instead of 8.5 mg/100 mL if this were true for individuals who have ingested large dose. The patient reported by Morley and Wynne would have had serum barbiturate levels of 50 mg/100 mL, which would have been fatal.[57]
History
Primidone's effectiveness for epilepsy was first demonstrated in 1949 by Yule Bogue.[6] It was introduced a year later by the Imperial Chemical Industry (ICI), now known as AstraZeneca in the United Kingdom[62][89] and Germany.[63] In 1952, it was approved in the Netherlands.[59] That same year, Drs. Handley and Stewart demonstrated its effectiveness in the treatment of patients who failed to respond to other therapies; it was noted to be more effective in people with idiopathic generalized epilepsy than in people whose epilepsy had a known cause.[6] Dr. Whitty noted in 1953 that it benefitted patients with psychomotor epilepsy, who were often treatment-resistant. Toxic effects were reported to be mild.[7] That same year, it was approved in France.[90] Primidone was introduced in 1954 under the brandname Mysoline by Wyeth in the United States.[91]
The first report associating it with megaloblastic anemia came in 1954 from Drs. Chalmers and Boheimer.[92] Between 1954 and 1957, twenty-one cases of megaloblastic anemia associated with primidone and/or phenytoin were reported.[93] Most cases were due to folic acid deficiency; however, there was one that only responded to B12 therapy[92] and one that required Vitamin C.[93] Some cases were associated with deficient diets; one patient ate mostly bread and butter,[92] another ate bread, buns, and hard candy, and another could rarely be persuaded to eat in the hospital.[93] The idea that folic acid deficiency could cause megaloblastic anemia was not new. What was new was the idea that drugs could cause this in well-nourished people with no intestinal abnormalities.[92] In many cases, it was not clear which drug had caused it.[94] It was speculated that this might be related to the structural similarity between folic acid, phenytoin, phenobarbital, and primidone.[95] Folic acid had been found to alleviate the symptoms of megaloblastic anemia in the 1940s, not long after it was discovered, but the typical patient only made a full recovery—cessation of CNS and PNS symptoms as well as anemia—on B12 therapy.[96] Five years earlier, folic acid deficiency was linked to birth defects in rats.[97] Primidone was seen by some as too valuable to withhold based on the slight possibility of this rare side effect[92] and by others as dangerous enough to be withheld unless phenobarbital or some other barbiturate failed to work for this and other reasons (i.e., reports of permanent psychosis.[98]
In Europe, up until 1963, it was not uncommon to prescribe primidone and phenobarbital in combination, often with a stimulant. They were believed to be the most useful for seizures occurring upon awakening, while phenytoin was the most useful for nocturnal seizures. Primidone and phenobarbital were prescribed in combination with phenytoin in diffuse epilepsies. They were third and fourth line-agents, respectively, in the treatment of partial seizures. By 1963, carbamazepine was marketed in most of Europe. It soon became clear that its efficacy in generalized tonic-clonic seizures was the same as phenytoin, that its ability to control partial seizures was superior, along with its tolerability. Sodium valproate was approved in France in 1967. Because the doses were so low (200–400 mg/day), it was viewed as a moderately effective anticonvulsant whose best quality was its nonsedating nature. In spite of the availability of carbamazepine and valproate, physicians practicing in Mediterranean countries still preferred phenobarbital. Other medications were seen as not usually necessary. Phenytoin was to be used as adjunctive therapy only.[90] In spite of these advances, primidone was still considered to be a "sheet-anchor" anticonvulsant in the United Kingdom as late as 1969, along with phenobarbital and phenytoin, for the treatment of pediatric epilepsy in spite of its side effects[99] and one of two drugs (the other being sultiame) that were tried in adult patients if a combination of phenytoin and phenobarbital failed to control seizures. A review published that same year stated that carbamazepine did not live up to the claims of those who advocated its use in epilepsy.[100]
In 1968, a Dr. Meadow encountered six babies with cleft lip and palate in addition to other congenital abnormalities whose mothers had been taking anticonvulsants. Meadow wrote a letter in The Lancet asking for cases of cleft lip and palate in babies whose mothers had taken anticonvulsants. That same year, Milunsky, Graef, and Gaynor reported cases of cleft lip and palate associated with attempted abortion with methotrexate and aminopterin, which are folic acid antagonists.[101] While it was widely accepted by 1969 that these drugs could interfere with folic acid and that folic acid supplementation might have beneficial somatic effects, it was believed that folic acid supplementation could exacerbate seizures; this included the routine supplements given to pregnant women to prevent megaloblastic anemia.[100][102] By 1970, the doctor had collected thirty-two cases. Sixteen of them were born to women taking primidone. 25% of the thirty-two cases had congenital heart defects; the reported rate in cleft lip and palate was 3-5%. Meadow emphasized that there was no proof of an association, the immense value of anticonvulsants and the probably small odds of any one epileptic woman having a child with a congenital abnormality.[101] Roman and Caratzali reported in 1971 that the offspring of mice treated with primidone had more abnormal bone metaphases than controls; this was due to chromosomal lesions.[103] By the mid-1970s, it was obvious that this antagonistic effect of primidone was not due to the inhibition of dihydrofolate reductase, the enzyme responsible for the reduction of dihydrofolic acid to tetrahydrofolic acid, but rather to defective folate metabolism.[45]
Carbamazepine was approved in the United States for the treatment of adult epilepsy in 1974. Its lack of sedating properties relative to phenobarbital and lack of somatic effects relative to phenytoin generated much interest.[104] Within two years, primidone was no longer seen as the drug of choice for psychomotor epilepsy in the United States. This was because while carbamazepine and primidone are of roughly equal effectiveness, the former is less likely to cause sedation and cognitive impairment. Also, primidone has a greater tendency to cause undesirable psychiatric side effects compared with carbamazepine, which was noted to lessen pre-existing depressive symptoms.[12] By 1978, it looked as if its superior side effect profile would increase its use in epilepsy in the United States.[104] That same year, a review was published stating that primidone and phenobarbital were used less often in the United Kingdom due to their greater tendency to cause behavior disorders and interfere with learning in young children. Valproate was heralded by some as "the greatest thing since Greta Garbo" and carbamazepine had also risen in popularity.[105]
By 1980, primidone was seen as not worth mentioning as an option for childhood temporal lobe epilepsy by doctors in the United Kingdom.[106] In January 1981, Dr. O'Brien and colleagues reported that primidone had a positive effect on the essential tremor of one of their patients. This led them to initiate a twenty-person prospective study. Twelve of the participants responded well.[107] By 1984, valproic acid was the drug of choice for juvenile myoclonic epilepsy[108] and not the equally effective primidone.[109] However, as late as 1985, primidone was still one of the most widely used anticonvulsants.[13] At the close of the 1980s, primidone was still the preferred anticonvulsant for complex partial seizures in Germany.[90] In 1989, Dainippon Pharmaceutical launched Exegran (zonisamide), the first new, chemically unique, non-benzodiazepine anticonvulsant in decades.[110]
In 1990, primidone, along with phenobarbital, was a second-line agent in partial epilepsy with or without secondarily generalized tonic-clonic seizures and was one of four agents (the others being carbamazepine, phenytoin and phenobarbital) that was used along with ethosuximide or a benzodiazepine for any absence or myoclonic seizures when valproate failed to control tonic-clonics (at least in the United States).[111] After zonisamide, other new anticonvulsants came onto the market: felbamate, gabapentin, lamotrigine, and vigabatrin. All four were structurally distinct both from other anticonvulsants already on the market. They all had larger protective indexes than conventional agents and unlike these agents, the new ones did not cause birth defects in laboratory animals or antagonize folic acid. They seemed to be relatively mild in terms of side effects. Out of all of them lamotrigine was the most similar to phenytoin in its pattern of efficacy. Felbamate was the most effective for Lennox-Gastaut syndrome and was seen as a second-line agent in juvenile myoclonic epilepsy after valproate. These new agents were aggressively marketed. In 1994, felbamate became the anticonvulsant of last resort after ten people out of 100,000 came down with aplastic anemia.[112]
By 1994, primidone was no longer one of the most widely used anticonvulsants. Phenytoin was still regarded as the drug of choice for partial seizures due to its long half-life and low cost; but for children, carbamazepine was seen as the best one due to phenytoin's effects on physical appearance.[112] Topiramate was approved two years later. It, along with the others, was mainly used in patients refractory to carbamazepine and valproate. These new agents were often described as having "innovative" and "selective" mechanisms of action; in reality, most of them also worked similarly to older agents.[113] On February 28, 1998, Élan Corporation, plc, bought the trademark and exclusive product distribution rights for Mysoline from Wyeth in Canada and the United States at a cost of $46 million and a royalty on future sales.[114] The actual manufacture and distribution was done by Athena Neurosciences; their name appeared on a Mysoline package information sheet dated June 1998.[115] On November 30, 1999, levetiracetam was approved for the adjunctive treatment of partial epilepsy in adults in the United States.[116]
By the year 2000, primidone was something that was prescribed in the event that the patient had tried all other anticonvulsants and was not a candidate for surgery in the United States.[117] In April 2001, Élan decided to concentrate its efforts towards Zanaflex, Zonegran, Skelaxin, Abelcet, Azactam, Maxipime, Myobloc, and Cutivate. Mysoline was rationalized along with many other products that did not meet "certain commercial criteria."[118] Yamanouchi Pharma Technologies, a Palo Alto-based subsidiary of Yamanouchi Pharmaceutical Co., Ltd,[119] manufactured the actual drug.[120] By 2003, most of the people taking primidone for epilepsy were elderly people who had been taking the drug for many years.[121] In July 2004, Acorus Therapeutics Ltd. took over the manufacture and distribution of Mysoline from AstraZeneca[122] February 3, 2005: almost four years after acquiring it from Elan, Xcel was acquired by Valeant Pharmaceuticals International.[123] On April 1, 2005, Yamanouchi merged with Fujisawa Pharmaceutical Co., Ltd to form Astellas Pharma.[124] As of 2005, it is widely used in the treatment of many forms of epilepsy in developing countries.[50]
Available forms
Primidone is available as a 250 mg/5mL suspension, and in the form of 50 mg, 125 mg, and 250 mg tablets. It is also available in a chewable tablet formulation in Canada.[125]
It is marketed as several different brands including Mysoline (Canada,[126] Ireland,[127] Japan,[128] the United Kingdom,[129] and the United States[126]), Prysoline (Israel, Rekah Pharmaceutical Products, Ltd.),[130] Apo-Primidone,[125][131] Liskantin (Germany, Desitin),[132] Resimatil (Germany, Sanofi-Synthélabo GmbH),[133] Mylepsinum (Germany, AWD.pharma GmbH & Co., KG).,[134] and Sertan (Hungary, 250 mg tablets, ICN Pharmaceuticals Inc.)
Primidone has been available in the United States as only a tablet that's only a generic drug and only from Lannett since 1978.[135]
References
- 1 2 3 Ochoa, Juan G; Riche, Willise. (2005). "Antiepileptic Drugs: An Overview". eMedicine. eMedicine, Inc. Retrieved 2005-07-02.
- ↑ CDER, U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES (2003–2005). "Primidone (Mysoline)". Pharmacology Guide for Brain Injury Treatment. Brain Injury Resource Foundation. Retrieved 2005-07-02.
- ↑ Yale Medical School, Department of Laboratory Medicine (1998). "Therapeutic Drug Levels". YNHH Laboratory Manual - Reference Documents. Yale Medical School. Retrieved 2005-07-13.
- 1 2 Acorus Therapeutics, Ltd. (2005). "Mysoline 250 mg Tablets". electronic Medicines Compendium. Datapharm Communications and the Association of the British Pharmaceutical Industry (ABPI). Retrieved 2006-03-08.
- ↑ Broadley, Marissa A. (200). "Juvenile Myoclonic Epilepsy of Janz (JME)". The Childhood Seizure e-Book. Valhalla, New York. Retrieved 2005-07-03.
- 1 2 3 Williams, Denis (1 August 1956). "Treatment of Epilepsy with Mysoline". Proceedings of the Royal Society of Medicine. 49 (8): 589–91. PMC 1889099
 . PMID 13359420.
. PMID 13359420. - 1 2 Whitty, C. W. (September 5, 1953). "Value of primidone in epilepsy". British Medical Journal. 2 (4835): 540–1. doi:10.1136/bmj.2.4835.540. PMC 2029655
 . PMID 13082031.
. PMID 13082031. - ↑ Livingston, Samuel; Don Petersen (February 16, 1956). "Primidone (mysoline) in the treatment of epilepsy; results of treatment of 486 patients and review of the literature". New England Journal of Medicine. 254 (7): 327–9. doi:10.1056/NEJM195602162540706. PMID 13288784.
- ↑ Smith, Bernard H.; Francis L. McNaughton (May 1953). "Mysoline, a new anticonvulsant drug; its value in refractory cases of epilepsy.|titlhoward stern babba booey e = Mysoline, A new Anticonvulsant: Its Value in Refractory Cases of Epilepsy". Canadian Medical Association Journal. 68 (5): 464–7. PMC 1822778
 . PMID 13042720.
. PMID 13042720. - ↑ Powell, C.; Painter MJ; Pippenger CE (October 1984). "Primidone therapy in refractory neonatal seizures". Journal of Pediatrics. 105 (4): 651–4. doi:10.1016/S0022-3476(84)80442-4. PMID 6481545.
- ↑ Kagitani-Shimono, Kuriko; Imai Katsumi; Okamoto Nobuhiko; Ono Jiro; Okada Shintaro (January 2002). "Unverricht-Lundborg disease with cystatin B gene abnormalities". Pediatric Neurology. 26 (1): 55–60. doi:10.1016/S0887-8994(01)00336-8. PMID 11814737.
- 1 2 3 4 5 Rodin, Ernst A.; Rim CS; Kitano H; Lewis R; Rennick PM (1976). "A comparison of the effectiveness of primidone versus carbamazepine in epileptic outpatients". The Journal of Nervous and Mental Disease. 163 (1): 41–6. doi:10.1097/00005053-197607000-00006. PMID 819630.
- 1 2 3 4 5 6 7 8 9 10 Mattson RH, Cramer JA, Collins JF, Smith DB, Delgado-Escueta AV, Browne TR, Williamson PD, Treiman DM, et al. (July 8, 1985). "Comparison of carbamazepine, phenobarbital, phenytoin, and primidone in partial and secondarily generalized tonic-clonic seizures". New England Journal of Medicine. 313 (3): 145–51. doi:10.1056/NEJM198507183130303. PMID 3925335.
- 1 2 3 4 5 Hermanns, Guido; Soheyl Noachtar; Ingrid Tuxhorn; Hans Holthausen; Alois Ebner; Peter Wolf (July 1996). "Systematic Testing of Medical Intractability for Carbamazepine, Phenytoin, and Phenobarbital or Primidone in Monotherapy for Patients Considered for Epilepsy Surgery". Epilepsia. 37 (7): 675–9. doi:10.1111/j.1528-1157.1996.tb00632.x. PMID 8681900.
- 1 2 3 4 5 Smith, D. B.; Richard H. Mattson; J. A. Cramer; J. F. Collins; R. A. Novelly; B. Craft (1987). "Results of a nationwide Veterans Administration Cooperative Study comparing the efficacy and toxicity of carbamazepine, phenobarbital, phenytoin, and primidone". Epilepsia. 28 (Suppl 3): S50–8. doi:10.1111/j.1528-1157.1987.tb05778.x. PMID 3319543.
- 1 2 3 4 Gruber, C. M., Jr.; J. T. Brock; M. Dyken (January–February 1962). "Comparison of the effectiveness of phenobarital, mephobarbital, primidone, diphenylhydantoin, ethotoin, metharbital, and methylphenylethylhydantoin in motor seizures". Clinical Pharmacology and Therapeutics. 3: 23–8. PMID 13902356.
- 1 2 White, P. T.; Plott D; Norton J (January 1966). "Relative anticonvulsant potency of primidone; a double blind comparison". Archives of Neurology. 14 (1): 31–5. doi:10.1001/archneur.1966.00470070035004. PMID 5320823.
- 1 2 Zesiewicz TA, Elble R, Louis ED, Hauser RA, Sullivan KL, Dewey RB, Ondo WG, Gronseth GS, Weiner WJ (June 28, 2005). "Practice Parameter: Therapies for essential tremor: Report of the Quality Standards Subcommittee of the American Academy of Neurology". Neurology. 64 (12): 2008–20. doi:10.1212/01.WNL.0000163769.28552.CD. PMID 15972843. Retrieved 2007-08-11.
- ↑ DeSilvey DL; Moss AJ (July 1980). "Primidone in the treatment of the long QT syndrome: QT shortening and ventricular arrhythmia suppression". Annals of Internal Medicine. 93 (1): 53–4. doi:10.7326/0003-4819-93-1-53. PMID 7396315.
- ↑ Lan, Y. W. (December 1986). "[Primidone in the treatment of long Q-T syndrome. Clinical analysis of 4 cases]". Zhonghua Xin Xue Guan Bing Za Zhi (Chinese Journal of Cardiovascular Diseases) (in Chinese). 14 (6): 330–2, 380. PMID 3582153.
- ↑ Loukeris, Konstantinos; Davide Mauri; Padelis Pazarlis (October 2002). "QT length and heart function in primidone hypocalcaemia" (PDF). Acta Cardiologica. 57 (5): 367–9. doi:10.2143/AC.57.5.2005455. PMID 12405576.
- ↑ Monroe RR, Wise SP (1965). "Combined phenothiazine, chlordiazepoxide and primidone therapy for uncontrolled psychotic patients" (PDF). American Journal of Psychiatry. 122 (6): 694–8. doi:10.1176/appi.ajp.122.6.694 (inactive 2015-01-01). PMID 5320821. Retrieved 2007-02-21.
- ↑ Monroe, R. R. (February 1975). "Anticonvulsants in the treatment of aggression". Journal of Nervous and Mental Disease. 160 (2–1): 119–26. doi:10.1097/00005053-197502000-00006. PMID 1117287.
- ↑ Hayes, S. G. (March 1993). "Barbiturate anticonvulsants in refractory affective disorders". Annals of Clinical Psychiatry. 5 (1): 35–44. doi:10.3109/10401239309148922. PMID 8348197.
- ↑ Brown GM; Stone GH; Rathbone MP (October 9, 1993). "Primidone and rapid cycling affective disorders". The Lancet. 342 (8876): 925. doi:10.1016/0140-6736(93)91972-O. PMID 8105181.
- 1 2 Schaffer LC; Schaffer CB; Caretto J (June 1999). "The use of primidone in the treatment of refractory bipolar disorder". Annals of Clinical Psychiatry. 11 (2): 61–6. doi:10.3109/10401239909147050. PMID 10440522.
- ↑ Bergouignan, M. (October 1957). "[Recent developments in the medical treatment of essential trigeminal neuralgia: importance of various anti-epileptic medication.]". Gazette Médicale de France (in French). 64 (19): 1571–2 passim. PMID 13480440.
- ↑ Stuttgen, G. (March 1973). "Toxic epidermal necrolysis provoked by barbiturates". British Journal of Dermatology. 88 (3): 291–3. doi:10.1111/j.1365-2133.1973.tb07551.x. PMID 4541299.
- ↑ Lorber, John (July 26, 1958). "Primidone Treatment of Athetosis in Children". British Medical Journal. 2 (5090): 208. doi:10.1136/bmj.2.5090.208. PMC 2026118
 . PMID 13560827.
. PMID 13560827. - ↑ Thorn, I. (June 1962). "Primidone and chlordiazepoxide in cerebral palsy". Developmental Medicine and Child Neurology. 4 (3): 325–7. doi:10.1111/j.1469-8749.1962.tb03175.x. PMID 13921015.
- ↑ National Office of Animal Health. "Compendium of Veterinary Medicine". Retrieved 2007-03-19.
- ↑ The Pig Site. "Savaging of Piglets". Retrieved 2007-03-19.
- 1 2 3 4 5 "Summary of Product Characteristics" (PDF). Official Acorus Therapeutics Site. Acorus Therapeutics. 2007-06-01. pp. 3–4. Retrieved 2007-10-12.
- 1 2 Hart, M. G.; G. Hooper (July 2005). "Clinical associations of Dupuytren's disease". Postgraduate Medical Journal. 81 (957): 425–428. doi:10.1136/pgmj.2004.027425. PMC 1743313
 . PMID 15998816. Retrieved 2007-03-07.
. PMID 15998816. Retrieved 2007-03-07. - ↑ Critchley EM, Vakil SD, Hayward HW, Owen VM (1976). "Dupuytren's disease in epilepsy: result of prolonged administration of anticonvulsants". Journal of Neurology, Neurosurgery, and Psychiatry. 39 (5): 498–503. doi:10.1136/jnnp.39.5.498. PMC 492313
 . PMID 932769.
. PMID 932769. - ↑ Schwaninger, Markus; Ringleb, P; Winter, R; Kohl, B; Fiehn, W; Rieser, PA; Walter-Sack, I (March 1999). "Elevated plasma concentrations of homocysteine in antiepileptic drug treatment" (PDF). Epilepsia. 40 (3): 345–350. doi:10.1111/j.1528-1157.1999.tb00716.x. PMID 10080517. Retrieved 2007-03-16.
- ↑ Reynolds, Jr., N. C.; Miska, R. M. (April 1981). "Safety of anticonvulsants in hepatic porphyrias". Neurology. 31 (4): 480–4. doi:10.1212/wnl.31.4.480. PMID 7194443.
- ↑ Arif H, Buchsbaum R, Weintraub D, Koyfman S, Salas-Humara C, Bazil CW, Resor SR, Hirsch LJ (May 15, 2007). "Comparison and predictors of rash associated with 15 antiepileptic drugs". Neurology. 68 (20): 1701–9. doi:10.1212/01.wnl.0000261917.83337.db. PMID 17502552. Retrieved 2007-09-25.
- 1 2 3 Pack, A. M.; M. J. Morrell (2001). "Adverse effects of antiepileptic drugs on bone structure: epidemiology, mechanisms and therapeutic implications". CNS Drugs. 15 (8): 633–42. doi:10.2165/00023210-200115080-00006. PMID 11524035.
- 1 2 3 Valsamis, Helen A; Surender K Arora; Barbara Labban; Samy I McFarlane (September 6, 2006). "Antiepileptic drugs and bone metabolism". Nutrition & Metabolism. 3 (36): 36. doi:10.1186/1743-7075-3-36. PMC 1586194
 . PMID 16956398. Retrieved 2007-03-28.
. PMID 16956398. Retrieved 2007-03-28. - 1 2 Harrington, M. G.; H. M. Hodkinson (July 1987). "Anticonvulsant drugs and bone disease in the elderly". Journal of the Royal Society of Medicine. 80 (7): 425–427. PMC 1290903
 . PMID 3656313.
. PMID 3656313. - ↑ "Mysoline". RxList. p. 3. Retrieved 2007-03-11.
- ↑ Schick, Paul (2005). "Megaloblastic Anemia". eMedicine. Retrieved 2005-08-15.
- ↑ Reynolds, E. H.; J. F. Hallpike; B. M. Phillips; D. M. Matthews (September 1965). "Reversible absorptive defects in anticonvulsant megaloblastic anaemia". Journal of Clinical Pathology. 18 (5): 593–598. doi:10.1136/jcp.18.5.593. PMC 473011
 . PMID 5835440.
. PMID 5835440. - 1 2 Girdwood, R. H. (1976). "Drug-induced anaemias". Drugs. 11 (5): 394–404. doi:10.2165/00003495-197611050-00003. PMID 782836.
- 1 2 3 4 O'Brien, M. D.; S. K. Gilmour-White (2005). "Management of epilepsy in women". Postgraduate Medical Journal. 81 (955): 278–285. doi:10.1136/pgmj.2004.030221. PMC 1743264
 . PMID 15879038. Retrieved 2007-09-16.
. PMID 15879038. Retrieved 2007-09-16. - 1 2 Hernandez-Diaz S, S; Werler MM; Walker AM; Mitchell AA. (2000). "Folic acid antagonists during pregnancy and the risk of birth defects". New England Journal of Medicine. 343 (22): 1608–14. doi:10.1056/NEJM200011303432204. PMID 11096168.
- ↑ Biale, Y; H. Lewenthal (1984). "Effect of folic acid supplementation on congenital malformations due to anticonvulsive drugs". European Journal of Obstetrics, Gynecology, and Reproductive Biology. 18 (4): 211–6. doi:10.1016/0028-2243(84)90119-9. PMID 6519344.
- ↑ Bruno, M. K.; C. L. Harden (January 2002). "Epilepsy in Pregnant Women". Current Treatment Options in Neurology. 4 (1): 31–40. doi:10.1007/s11940-002-0003-7. PMID 11734102.
- 1 2 Lopez-Gomez, M; J. Ramirez-Bermudez; C. Campillo; A. L. Sosa; M. Espinola; I. Ruiz (May 2005). "Primidone is associated with interictal depression in patients with epilepsy". Epilepsy & Behavior. 6 (3): 413–6. doi:10.1016/j.yebeh.2005.01.016. PMID 15820351.
- ↑ Stores, G. (October 1975). "Behavioural effects of anti-epileptic drugs". Developmental Medicine and Child Neurology. 17 (5): 647–58. doi:10.1111/j.1469-8749.1975.tb03536.x. PMID 241674.
- ↑ Herranz, J. L.; J. A. Armijo; R. Arteaga (November–December 1988). "Clinical side effects of phenobarbital, primidone, phenytoin, carbamazepine, and valproate during monotherapy in children". Epilepsia. 29 (6): 794–804. doi:10.1111/j.1528-1157.1988.tb04237.x. PMID 3142761.
- ↑ Sher, A.; J. M. Andersen; S. C. Bhatia (July–August 1983). "Primidone-induced catatonic schizophrenia". Drug Intelligence & Clinical Pharmacy. 17 (7–8): 551–2. PMID 6872851.
- ↑ Schlienger, Raymond G.; Shear, Neil H. (1998). "Antiepileptic drug hypersensitivity syndrome" (PDF). Epilepsia. 39 (Suppl 7): S3–7. doi:10.1111/j.1528-1157.1998.tb01678.x. PMID 9798755. Retrieved 2007-01-20.
- ↑ Katano H, Fukushima T, Karasawa K, Sugiyama N, Ohkura A, Kamiya K (2002). "Primidone-induced hyperammonemic encephalopathy in a patient with cerebral astrocytoma" (PDF). Journal of Clinical Neuroscience. 9 (1): 79–81. doi:10.1054/jocn.2001.1011. PMID 11749025.
- ↑ Langlands, A. O.; N. Maclean; J. G. Pearson; E. R. Williamson (January 28, 1967). "Lymphadenopathy and megaloblastic anaemia in patient receiving primidone". British Medical Journal. 1 (5534): 215–217. doi:10.1136/bmj.1.5534.215. PMC 1840532
 . PMID 4959849.
. PMID 4959849. - 1 2 3 4 5 6 Kappy, Michael S.; Jerome Buckley (April 1969). "Primidone intoxication in a child". Archives of Disease in Childhood. 44 (234): 282–4. doi:10.1136/adc.44.234.282. PMC 2020038
 . PMID 5779436.
. PMID 5779436. - 1 2 3 4 5 Brillman, J.; B. B. Gallagher; R. H. Mattson (March 1974). "Acute primidone intoxication". Archives of Neurology. 30 (3): 255–8. doi:10.1001/archneur.1974.00490330063011. PMID 4812959.
- 1 2 3 4 5 van Heijst, A. N.; W. de Jong; R. Seldenrijk; A. van Dijk (June 1983). "Coma and crystalluria: a massive primidone intoxication treated with haemoperfusion". Journal of Toxicology. Clinical Toxicology. 20 (4): 307–18. doi:10.3109/15563658308990598. PMID 6655772.
- 1 2 3 Bailey, D. N.; P. I. Jatlow (November 1972). "Chemical analysis of massive crystalluria following primidone overdose". American Journal of Clinical Pathology. 58 (5): 583–9. PMID 4642162.
- ↑ Turner, C. R. (October 1980). "Primidone intoxication and massive crystalluria". Clinical Pediatrics. 19 (10): 706–7. doi:10.1177/000992288001901015. PMID 7408374.
- 1 2 3 4 Dotevall, Gerhard; Birger Herner (August 24, 1957). "Treatment of Acute Primidone Poisoning with Bemegride and Amiphenazole". British Medical Journal. 2 (5042): 451–2. doi:10.1136/bmj.2.5042.451. PMC 1961943
 . PMID 13446511.
. PMID 13446511. - 1 2 3 Fazekas, I. Gy.; B. Rengei (January 1960). "Tödliche Vergiftung (Selbstmord) mit Mysoline und Phenobarbiturat" (PDF). Archives of Toxicology (in German). 18 (4): 213–23. doi:10.1007/BF00577226. PMID 13698457. Retrieved 2007-11-05.
- ↑ Ajax, E. T. (October 1966). "An unusual case of primidone intoxication". Diseases of the Nervous System. 27 (10): 660–1. PMID 5919666.
- 1 2 "Primidone". The Merck Manual's Online Medical Library. Lexi-Comp. Retrieved 2007-10-04.
- 1 2 Desta, Zeruesenay; Nadia V. Soukhova; David A. Flockhart (February 2001). "Inhibition of Cytochrome P450 (CYP450) Isoforms by Isoniazid: Potent Inhibition of CYP2C19 and CYP3A". Antimicrobial Agents and Chemotherapy. 45 (2): 382–92. doi:10.1128/AAC.45.2.382-392.2001. PMC 90302
 . PMID 11158730.
. PMID 11158730. - ↑ Theis JG, Koren G, Daneman R, Sherwin AL, Menzano E, Cortez M, Hwang P (1997). "Interactions of clobazam with conventional antiepileptics in children". Journal of Child Neurology. 12 (3): 208–13. doi:10.1177/088307389701200311. PMID 9130097.
- ↑ Browne, Thomas R.; Robert G. Feldman; Robert A. Buchanan RA; Nancy C. Allen; L. Fawcett-Vickers; GK Szabo; GF Mattson; SE Norman; DJ Greenblatt (April 1983). "Methsuximide for complex partial seizures: efficacy, toxicity, clinical pharmacology, and drug interactions". Neurology. 33 (4): 414–8. doi:10.1212/WNL.33.4.414. PMID 6403891.
- ↑ Spina, Edoardo; Francesco Pisani; Emilio Perucca (September 1996). "Clinically significant pharmacokinetic drug interactions with carbamazepine. An update". Clinical Pharmacokinetics. 31 (3): 198–214. doi:10.2165/00003088-199631030-00004. PMID 8877250.
- ↑ GlaxoSmithKline (2005). "LAMICTAL Prescribing Information" (PDF). Retrieved 2006-03-14.
- 1 2 Spina, Edoardo; Emilio Perucca (February 2002). "Clinical Significance of Pharmacokinetic Interactions Between Antiepileptic and Psychotropic Drugs". Epilepsia. 43 (Suppl 2): 37–44. doi:10.1046/j.1528-1157.2002.043s2037.x. PMID 11903482. Retrieved 2007-10-07.
- 1 2 Perucca, E.; A. Hedges; K. A. Makki; M. Ruprah; J. F. Wilson; A. Richens (1984). "A comparative study of the relative enzyme inducing properties of anticonvulsant drugs in epileptic patients" (PDF). British Journal of Clinical Pharmacology. 18 (3): 401–10. doi:10.1111/j.1365-2125.2004.02311.x. PMC 1463658
 . PMID 6435654. Retrieved 2007-03-23.
. PMID 6435654. Retrieved 2007-03-23. - ↑ Young MC, Hughes IA (1991). "Loss of therapeutic control in congenital adrenal hyperplasia due to interaction between dexamethasone and primidone". Acta Paediatrica Scandinavica. 80 (1): 120–4. doi:10.1111/j.1651-2227.1991.tb11744.x. PMID 2028784.
- ↑ Tempelhoff R, Modica PA, Spitznagel EL (1990). "Anticonvulsant therapy increases fentanyl requirements during anaesthesia for craniotomy". Canadian Journal of Anesthesia. 37 (3): 327–32. doi:10.1007/BF03005584. PMID 2108815.
- ↑ "Mysoline: Clinical Pharmacology". RxList. Retrieved 2007-10-07.
- ↑ MacDonald, R. L.; K. M. Kelly (1995). "Antiepileptic drug mechanisms of action". Epilepsia. 36 (Suppl 2): S2–12. doi:10.1111/j.1528-1157.1995.tb05996.x. PMID 8784210.
- ↑ Calzetti, S.; L. J. Findley; F. Pisani; A. Richens (October 1981). "Phenylethylmalonamide in essential tremor. A double-blind controlled study". Journal of Neurology, Neurosurgery, and Psychiatry. 44 (10): 932–934. doi:10.1136/jnnp.44.10.932. PMC 491180
 . PMID 7031184. Retrieved 2007-02-12.
. PMID 7031184. Retrieved 2007-02-12. - ↑ Gatti, G.; M. Furlanut; E. Perrucca (2001-07-01). "Interindividual variability in the metabolism of anti-epileptic drugs and its clinical application". In Gian Maria Pacifici and Olavi Pelkonen (eds.). Interindividual Variability in Human Drug Metabolism. CRC Press. pp. 168. ISBN 0-7484-0864-9.
- ↑ Nau H; Jesdinsky D; Wittfoht W (1980). "Microassay for primidone and its metabolites phenylethylmalondiamide, phenobarbital and p-hydroxyphenobarbital in human serum, saliva, breast milk and tissues by gas chromatography—mass spectrometry using selected ion monitoring". Journal of Chromatography B. 182 (1): 71–9. doi:10.1016/S0378-4347(00)81652-7. PMID 7380904.
- ↑ Alvin J; Goh E; Bush MT (July 1975). "Study of the hepatic metabolism of primidone by improved methodology". Journal of Pharmacology and Experimental Therapeutics. 194 (1): 117–25. PMID 1151744.
- ↑ Hooper WD; Treston AM; Jacobsen NW; Dickinson RG; Eadie MJ (November–December 1983). "Identification of p-hydroxyprimidone as a minor metabolite of primidone in rat and man". Drug Metabolism and Disposition. 11 (6): 607–10. PMID 6140148.
- ↑ Lee, Anna M.; Sharon Miksys; Rachel F. Tyndale (July 2006). "Phenobarbital increases monkey in vivo nicotine disposition and induces liver and brain CYP2B6 protein". British Journal of Pharmacology. 148 (6): 786–4. doi:10.1038/sj.bjp.0706787. PMC 1617079
 . PMID 16751792. Retrieved 2007-10-07.
. PMID 16751792. Retrieved 2007-10-07. - 1 2 Kojima, Koki; Kiyoshi Nagata; Tsutomu Matsubara; Yasushi Yamazoe (August 2007). "Broad but distinct role of pregnane x receptor on the expression of individual cytochrome p450s in human hepatocytes". Drug Metabolism & Pharmacokinetics. 22 (4): 276–86. doi:10.2133/dmpk.22.276. PMID 17827782. Retrieved 2007-10-07.
- ↑ Madan A, Graham RA, Carroll KM, Mudra DR, Burton LA, Krueger LA, Downey AD, Czerwinski M, Forster J, Ribadeneira MD, Gan LS, LeCluyse EL, Zech K, Robertson P, Koch P, Antonian L, Wagner G, Yu L, Parkinson A (April 2003). "Effects of Prototypical Microsomal Enzyme Inducers on Cytochrome P450 Expression in Cultured Human Hepatocytes". Drug Metabolism and Disposition. 31 (4): 421–31. doi:10.1124/dmd.31.4.421. PMID 12642468. Retrieved 2007-10-07.
- ↑ Li, Chien-Chun; Chong-Kuei Lii; Kai-Li Liu; Jaw-Ji Yang; Haw-Wen Chen (August 23, 2007). "DHA down-regulates phenobarbital-induced cytochrome P450 2B1 gene expression in rat primary hepatocytes by attenuating CAR translocation". Toxicology and Applied Pharmacology. 225 (3): 329–36. doi:10.1016/j.taap.2007.08.009. PMID 17904175.
- ↑ Kobayashi, Kaoru; Saeko Yamagami; Tomoaki Higuchi; Masakiyo Hosokawa; Kan Chiba (April 2004). "Key structural features of ligands for activation of human pregnane X receptor". Drug Metabolism and Disposition. 32 (4): 468–72. doi:10.1124/dmd.32.4.468. PMID 15039302. Retrieved 2007-10-07.
- ↑ Battino D, Avanzini G, Bossi L, Croci D, Cusi C, Gomeni C, Moise A (1983). "Plasma levels of primidone and its metabolite phenobarbital: effect of age and associated therapy". Therapeutic Drug Monitoring. 5 (1): 73–9. doi:10.1097/00007691-198303000-00006. PMID 6845402.
- ↑ Martines C, Gatti G, Sasso E, Calzetti S, Perucca E (1990). "The disposition of primidone in elderly patients". British Journal of Clinical Pharmacology. 30 (4): 607–11. doi:10.1111/j.1365-2125.1990.tb03820.x. PMC 1368252
 . PMID 2291873.
. PMID 2291873. - ↑ Morley, D.; N. A. Wynne (January 12, 1957). "Acute Primidone Poisoning in a Child". British Medical Journal. 1 (5010): 90. doi:10.1136/bmj.1.5010.90. PMC 1974075
 . PMID 13383203.
. PMID 13383203. - 1 2 3 Loiseau, Pierre Jean-Marie (June 1999). "Clinical Experience with New Antiepileptic Drugs: Antiepileptic Drugs in Europe" (PDF). Epilepsia. 40 (Suppl 6): S3–8. doi:10.1111/j.1528-1157.1999.tb00925.x. PMID 10530675. Retrieved 2007-03-26.
- ↑ Wyeth. "Wyeth Timeline". About Wyeth. Retrieved 2007-11-11.
- 1 2 3 4 5 Newman, M. J. D.; D. W. Sumner (February 1957). "Megaloblastic anemia following the use of primidone" (PDF). Blood. 12 (2): 183–8. PMID 13403983.
- 1 2 3 Kidd, Patrick; David L. Mollin (October 26, 1957). "Megaloblastic Anaemia and Vitamin-B12 Deficiency After Anticonvulsant Therapy". British Medical Journal. 2 (5051): 97–976. doi:10.1136/bmj.2.2689.97. PMC 1962638
 . PMID 13472024.
. PMID 13472024. - ↑ Fuld, H.; E. H. Moorhouse (May 5, 1956). "Observations on Megaloblastic Anaemias After Primidone". British Medical Journal. 1 (4974): 1021–3. doi:10.1136/bmj.1.4974.1021. PMC 1979778
 . PMID 13304415.
. PMID 13304415. - ↑ Girdwood, R. H.; J. A. R. Lenman (January 21, 1956). "Megaloblastic Anaemia Occurring During Primidone Therapy". British Medical Journal. 1 (4959): 146–7. doi:10.1136/bmj.1.4959.146. PMC 1978898
 . PMID 13276653.
. PMID 13276653. - ↑ Meyer, Leo M. (1 January 1947). "Folic Acid In The Treatment Of Pernicious Anemia" (PDF). Blood. 2 (1): 50–62. PMID 20278334. Retrieved 2007-08-27.
- ↑ Nelson, Marjorie M.; C. Willet Asling; Herbert M. Evans (1 September 1952). "Production of multiple congenital abnormalities in young by maternal pteroylglutamic acid deficiency during gestation" (PDF). Journal of Nutrition. 48 (1): 61–79. PMID 13000492. Retrieved 2008-01-06.
- ↑ Garland, Hugh (August 1957). "Drugs used in the management of epilepsy". Proceedings of the Royal Society of Medicine. 50 (8): 611–5. PMC 1889058
 . PMID 13465742.
. PMID 13465742. - ↑ Wilson, John (November 22, 1969). "Drug treatment of epilepsy in childhood". British Medical Journal. 4 (5681): 475–7. doi:10.1136/bmj.4.5681.475. PMC 1630558
 . PMID 4390959.
. PMID 4390959. - 1 2 Gibberd, F. B. (1 November 1969). "Epilepsy". British Medical Journal. 4 (5678): 281–4. doi:10.1136/bmj.4.5678.281. PMC 1629736
 . PMID 4390562.
. PMID 4390562. - 1 2 Meadow, S. R. (January 1970). "Congenital abnormalities and anticonvulsant drugs". Proceedings of the Royal Society of Medicine. 63 (1): 48–9. PMC 1810946
 . PMID 5417773.
. PMID 5417773. - ↑ Baumslag, Naomi; T. Edelstein; J. Metz (January 3, 1970). "Reduction of Incidence of Prematurity by Folic Acid Supplementation in Pregnancy". British Medical Journal. 1 (5687): 16–7. doi:10.1136/bmj.1.5687.16. PMC 1700896
 . PMID 5460838.
. PMID 5460838. - ↑ Roman, I. C.; A. Caratzali (October 23, 1971). "Effects of anticonvulsant drugs on chromosomes". British Medical Journal. 4 (5781): 234. doi:10.1136/bmj.4.5781.234-b. PMC 1799267
 . PMID 5115838.
. PMID 5115838. - 1 2 Schain RJ (March 1978). "Pediatrics-Epitomes of Progress: Carbamazepine (Tegretol) in the Treatment of Epilepsy". West. J. Med. 128 (3): 231–232. PMC 1238063
 . PMID 18748164.
. PMID 18748164. - ↑ Addy DP (1978). "Childhood epilepsy". British Medical Journal. 2 (6140): 811–2. doi:10.1136/bmj.2.6140.811. PMC 1607822
 . PMID 698744.
. PMID 698744. - ↑ "Prognosis of temporal lobe epilepsy in childhood.". British Medical Journal. 280 (6217): 812–3. March 22, 1980. doi:10.1136/bmj.280.6217.812. PMC 1600996
 . PMID 7370676.
. PMID 7370676. - ↑ O'Brien, M D; A R Upton and P A Toseland (January 17, 1981). "Benign familial tremor treated with primidone". British Medical Journal. 282 (6259): 178–80. doi:10.1136/bmj.282.6259.178. PMC 1503935
 . PMID 6779938.
. PMID 6779938. - ↑ Asconapé, J.; J. K. Penry (February 1984). "Some clinical and EEG aspects of benign juvenile myoclonic epilepsy". Epilepsia. 25 (1): 108–14. doi:10.1111/j.1528-1157.1984.tb04163.x. PMID 6420145.
- ↑ Janz, D. (November 1985). "Epilepsy with impulsive petit mal (juvenile myoclonic epilepsy)". Acta Neurologica Scandinavica. 72 (5): 449–59. doi:10.1111/j.1600-0404.1985.tb00900.x. PMID 3936330.
- ↑ Dainippon Sumitomo Pharma Co., Ltd. (2005). "Company History". Company Information. Dainippon Sumitomo Co., Ltd. Archived from the original on 2006-02-13. Retrieved 2005-11-12.
- ↑ Mattson, R. H. (December 1990). "Selection of drugs for the treatment of epilepsy". Seminars in Neurology. 10 (4): 406–13. doi:10.1055/s-2008-1063985. PMID 2287835.
- 1 2 Laxer, K. D. (September 1994). "Guidelines for treating epilepsy in the age of felbamate, vigabatrin, lamotrigine, and gabapentin". Western Journal of Medicine. 161 (3): 309–14. PMC 1011415
 . PMID 7975572.
. PMID 7975572. - ↑ Perucca, Emilio (1996). "The new generation of antiepileptic drugs: advantages and disadvantages". British Journal of Clinical Pharmacology. 42 (5): 531–43. doi:10.1111/j.1365-2125.1996.tb00046.x. PMID 8951184. Retrieved 2007-09-24.
- ↑ Élan Corporation, plc. "Product Acquisitions" (PDF). Annual Report Pursuant to Section 13 or 15(d) of The Securities Exchange Act of 1934 for the fiscal year ended: December 31, 1998. Archived from the original (PDF) on 2005-05-23. Retrieved 2005-07-03.
- ↑ Medscape. "Athena Neurosciences. Mysoline (primidone) package insert. South San Francisco, CA; June 1998.". Medscape: References. Retrieved 2005-07-03.
- ↑ U.S. Food and Drug Administration Center for Drug Evaluation and Research. "Drug Approval Package: Keppra (Levetiracetam) Tablets". Archived from the original on 2007-10-19. Retrieved 2007-11-14.
- ↑ Kanner, Andres M.; Jaime Parra; Marlis Frey (October 2000). "The "Forgotten" Cross-Tolerance Between Phenobarbital and Primidone: It Can Prevent Acute Primidone-Related Toxicity" (PDF). Epilepsia. 41 (10): 1310–4. doi:10.1111/j.1528-1157.2000.tb04610.x. PMID 11051127. Retrieved 2007-11-12.
- ↑ Élan Corporation, plc (2001). "2001 Annual Report and Form 20-F" (PDF). elan.com. p. 25. Archived from the original (PDF) on May 23, 2005. Retrieved 2005-07-03.
- ↑ Informagen (2000). "Yamanouchi Pharma Technologies, Inc. (YPT)". Resource Informagen. Retrieved 2005-07-03.
- ↑ "Mysoline Indications, Dosage, Storage, Stability". Primidone - RxList Monograph. Retrieved 2005-07-03.
- ↑ de Haan, G. J.; J. A. Carpay; C. A. van Donselaar (November 22, 2003). "Anti-epilepticum primidon binnenkort uit de handel: nu medicatie herzien / Antiepileptic primidone shortly to be withdrawn from sale: change medication now". Nederlands Tijdschrift voor Geneeskunde (in Dutch). 147 (47): 2325–6. PMID 14669538. Retrieved 2007-10-06.
- ↑ AstraZeneca (2004). "Mysoline, Mylepsinum (primidone) - anticonvulsant used to treat epilepsy". Retrieved 2005-07-03.
- ↑ KESQ NewsChannel 3 Palm Springs, CA (2005). "Valeant to buy Xcel Pharmaceuticals for $280 million". Archived from the original on September 27, 2007. Retrieved 2005-07-03.
- ↑ "Yamanouchi, Fujisawa Unite to Form Astellas - Canadian operation based in Markham, Ontario" (PDF). Retrieved 2005-07-03.
- 1 2 Schachter, Steven C. (February 2004). "Mysoline". Epilepsy.com. Epilepsy Therapy Development Project. Retrieved 2007-01-10.
- 1 2 "Valeant Pharmaceuticals International: Products". Archived from the original on 2005-06-01. Retrieved 2005-07-03.
- ↑ "Service List". Archived from the original on 15 May 2006. Retrieved 13 March 2006.
- ↑ Dainippon Sumitomo Pharma (2005). "Primidone 250 mg Tablets & Primidone 99.5% Powder" (PDF). Retrieved 13 March 2006.
- ↑ "Acorus Therapeutics Ltd. - Ordering - UK". acorus-therapeutics.com. Acorus Therapeutics. Archived from the original on 2005-04-07. Retrieved 2005-07-04.
- ↑ "Prysoline Tablets". The Israel Drug Registry. The State of Israel. 2005. Retrieved 2006-02-17.
- ↑ "APO-PRIMIDONE". Apotex. 2007-01-10. Retrieved 2007-01-10.
- ↑ "Liskantin". Desitin. Retrieved 2005-07-03.
- ↑ "Resimatil Tabletten". Deutsche Krankenversicherung AG. Retrieved 2005-07-03.
- ↑ "Mylepsinum Tabletten". Deutsche Krankenversicherung AG. Retrieved 2005-07-03.
- ↑ "Approval History". Drugs@FDA. United States Food and Drug Administration Center for Drug Evaluation and Research. Retrieved 17 February 2006.
Further reading
- "TR-476 Toxicology and Carcinogenesis Studies of Primidone (CAS No. 125-33-7) in F344/N Rats and B6C3F1 Mice (Feed Studies)". Department of Health and Human Services National Toxicology Program. Retrieved 2 July 2005.