Patellar dislocation
| Patellar dislocation | |
|---|---|
 | |
| Radiograph of a patient with patellar dislocation. Normally the patella projects over the distal femur. | |
| Classification and external resources | |
| eMedicine | article/90068 article/109263 |
| MeSH | D031222 |
Patellar dislocation is an injury of the knee, typically caused by a direct blow or a sudden twist of the leg.[1] It occurs when the patella (kneecap) slips out of its normal position in the patellofemoral groove, and generally causes intense pain with swelling of the knee.[1] Open or arthroscopic surgery may be used to repair damage, but are typically avoided since rates of re-injury, knee function, and patients' opinions do not differ much from conservative treatment.[2][3][4]
The patella generally dislocates laterally, and can be accompanied by acute pain and disability. Immediate reduction can be accomplished by hyperextension of the knee, and by providing a medialward pressure to move the patella back into the patellofemoral groove. Hyperextension of the knee on its own could possibly move the patella into place, because this motion locks the knee in place. When the knee is locked the ligaments are twisted and taut, allowing the muscles involved to relax and the patella to slide back into place.[5] If that does not work, a medical professional must manually perform an orthopedic reduction.[1] Swelling and impaired mobility follow patellar dislocation,[6] and a rehabilitation program of six to sixteen weeks is recommended whether or not the patient undergoes surgery.[3]
Young athletes suffer patellar dislocations more commonly than any other group,[7] and the average age of occurrences is 16–20 years.[8] Sports commonly associated with the injury involve sudden twisting motions of the knee and/or impact, such as soccer, gymnastics and ice hockey.[1] It can also occur when a person trips over an object or slips on a slick surface, especially if that person has predisposing factors.
Signs and symptoms
People often describe pain as being “inside the knee cap.” The leg tends to flex even when relaxed. In some cases, the injured ligaments involved in patellar dislocation do not allow the leg to flex almost at all.[1]
Risk factors
A predisposing factor is tightness in the tensor fasciae latae muscle and iliotibial tract in combination with a quadriceps imbalance between the vastus lateralis and vastus medialis muscles can play a large role. However individuals with larger Q angles are genetically more predisposed to this type of injury due to the increased lateral angle at which the femur and tibia meet.
Another cause of patellar symptoms is lateral patellar compression syndrome, which can be caused from lack of balance or inflammation in the joints.[9] The pathophysiology of the kneecap is complex, and deals with the osseous soft tissue or abnormalities within the patellofemoral groove. The patellar symptoms cause knee extensor dysplasia, and sensitive small variations affect the muscular mechanism that controls the joint movements.[10]
24% of patients whose patellas have dislocated have relatives who have experienced patellar dislocations.[1]
Athletic population
Patellar dislocation occurs in sports that involve rotating the knee. Direct trauma to the knee can knock the patella out of joint.[8]
Anatomical factors
People who have larger Q angles tend to be more prone to having knee injuries such as dislocations, due to the central line of pull found in the quadriceps muscles that run from the anterior superior iliac spine to the center of the patella. The range of a normal Q angle for men ranges from <15 degrees and for females <20 degrees, putting females at a higher risk for this injury.[11] An angle greater than 25 degrees between the patellar tendon and quadriceps muscle can predispose a person to patellar dislocation.[2]
In patella alta, the patella sits higher on the knee than normal.[2] Normal function of the VMO muscle stabilizes the patella. Decreased VMO function results in instability of the patella.[1]
Forces
When there is too much tension on the patella, the ligaments will weaken and be susceptible to tearing ligaments or tendons due to shear force or torsion force, which then displaces the kneecap from its origination. Another cause that patellar dislocation can occur is when the trochlear groove that has been completely flattened is defined as trochlear dysplasia.[12] Not having a groove because the trochlear bone has flattened out can cause the patella to slide because nothing is holding the patella in place.
Mechanism of injury
Patellar dislocations occur by:
- A direct impact that knocks the patella out of joint
- A twisting motion of the knee, or ankle
- A sudden lateral cut [1]
Anatomy of the knee
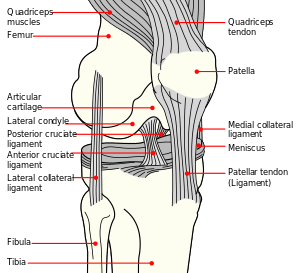
The patella is a triangular sesamoid bone which is embedded in tendon. It rests in the patellofemoral groove, an articular cartilage-lined hollow at the end of the thigh bone (femur) where the thigh bone meets the shin bone (tibia). Several ligaments and tendons hold the patella in place and allow it to move up and down the patellofemoral groove when the leg bends. The top of the patella attaches to the quadriceps muscle via the quadriceps tendon,[1] the middle to the vastus medialis obliquus and vastus lateralis muscles, and the bottom to the head of the tibia (tibial tuberosity) via the patellar tendon, which is a continuation of the quadriceps femoris tendon.[13] The medial patellofemoral ligament attaches horizontally in the inner knee to the adductor magnus tendon and is the structure most often damaged during a patellar dislocation. Finally, the lateral collateral ligament and the medial collateral ligament stabilize the patella on either side.[1] Any of these structures can sustain damage during a patellar dislocation.
Diagnosis

To assess the knee, a clinician can perform the patellar apprehension test by moving the patella back and forth while the patient flexes the knee at approximately 30 degrees.[6]
The patient can do the patella tracking assessment by making a single leg squat and standing, or by lying on his or her back with knee extended from flexed position. A patella that slips medially on early flexion is called the J sign, and indicates imbalance between the VMO and lateral structures.[14]
Prevention
The patella is a floating sesamoid bone held in place by the quadriceps muscle tendon and patellar tendon ligament. Exercises should strengthen quadriceps muscles such as rectus femoris, vastus intermedius, and vastus lateralis. However, tight and strong lateral quadriceps can be an underlying cause of patellar dislocation. If this is the case, it is advisable to strengthen the medial quadriceps, vastus medialis (VMO), and stretch the lateral muscles.[15] Exercises to strengthen quadriceps muscles include, but are not limited to, squats and lunges. Adding extra external support around the knee by using devices such as knee [orthotics] or athletic tape can help to prevent patellar dislocation and other knee-related injuries.[16] External supports, such as knee braces and athletic tape, work by providing movement in only the desired planes and help hinder movements that can cause abnormal movement and injuries. Women who wear high heels tend to develop short calf muscles and tendons. Exercises to stretch and strengthen calf muscles are recommended on a daily basis.[17]
Treatment

Two types of treatment options are typically available:
- Surgery
- Conservative treatment (rehabilitation and physical therapy)
Surgery may impede normal growth of structures in the knee, so doctors generally do not recommend knee operations for young people who are still growing.[3][4] There are also risks of complications, such as an adverse reaction to anesthesia or an infection.[2][3][4]
When designing a rehabilitation program, clinicians consider associated injuries such as chipped bones or soft tissue tears. Clinicians take into account the patient's age, activity level, and time needed to return to work and/or athletics. Doctors generally only recommend surgery when other structures in the knee have sustained severe damage, or specifically when there is:[3]
- Concurrent osteochondral injury
- Continued gross instability
- Palpable disruption of the medial patellofemoral ligament and the vastus medialis obliquus
- High-level athletic demands coupled with mechanical risk factors and an initial injury mechanism not related to contact
Supplements like glucosamine and NSAIDs can be used to minimize bothersome symptoms.[6]
Rehabilitation
An effective rehabilitation program reduces the chances of reinjury and of other knee-related problems such as patellofemoral pain syndrome and osteoarthritis. Rehabilitation focuses on maintaining strength and range of motion to reduce pain and maintain the health of the muscles and tissues around the knee joint.[6]
Epidemiology
Rate in the United States have been estimated to occur among an at-risk population of 1,774,210,081 people each year.[18] Incidence rates published in the American Journal of Sports Medicine for ages 10–17 were found to be about 29 per 100,000 persons per year, while the adult population average for this type of injury ranged between 5.8 and 7.0 per 100,000 persons per year.[19] The highest rates of patellar dislocation were found in the youngest age groups, while the rates declined with increasing ages. Females are more susceptible to patellar dislocation. Race is a significant factor for this injury, where Hispanics, African-Americans and Caucasians had slightly higher rates of patellar dislocation due to the types of athletic activity involved in: basketball (18.2%), soccer (6.9%), and football (6.9%), according to Brian Waterman.[18]
Lateral Patellar dislocation is common among the child population. Some studies suggest that the annual patellar dislocation rate in children is 43/100,000.[20] The treatment of the skeletally immature is controversial due to the fact that they are so young and are still growing. Surgery is recommended by some experts in order to repair the medial structures early, while others recommend treating it non operatively with physical therapy. If re-dislocation occurs then reconstruction of the medial patellofemoral ligament (MPFL) is the recommended surgical option.[21]
References
- 1 2 3 4 5 6 7 8 9 10 Dath, R; Chakravarthy, J; Porter, KM (2006). "Patella dislocations". Trauma. 8 (1): 5–11. doi:10.1191/1460408606ta353ra. ISSN 1460-4086.
- 1 2 3 4 Buchner M, Baudendistel B, Sabo D, Schmitt H (March 2005). "Acute traumatic primary patella dislocation: long-term results comparing conservative and surgical treatment". Clin J Sport Med. 15 (2): 62–6. doi:10.1097/01.jsm.0000157315.10756.14. PMID 15782048.
- 1 2 3 4 5 Shea KG, Nilsson K, Belzer J (2006). "Patellar dislocation in skeletally immature athletes". Operative Techniques in Sports Medicine. 14 (3): 188–196. doi:10.1053/j.otsm.2006.08.001.
- 1 2 3 Nikku R, Nietosvaara Y, Kallio PE, Aalto K, Michelsson JE (October 1997). "Operative versus closed treatment of primary dislocation of the patella. Similar 2-year results in 125 randomized patients". Acta Orthop Scand. 68 (5): 419–23. doi:10.3109/17453679708996254. PMID 9385238.
- ↑ Hirata, Isao (1974). The doctor and the athlete (2nd ed.). Philadelphia: J. B. Lippincott. pp. 227–228. ISBN 0-397-50330-X.
- 1 2 3 4 Brukner, P.; Khan, K. (2006). Clinical Sports Medicine (3rd ed.). McGraw-Hill.
- ↑ Palmu S, Kallio PE, Donell ST, Helenius I, Nietosvaara Y (March 2008). "Acute patellar dislocation in children and adolescents: a randomized clinical trial". J Bone Joint Surg Am. 90 (3): 463–70. doi:10.2106/JBJS.G.00072. PMID 18310694.
- 1 2 Atkin DM, Fithian DC, Marangi KS, Stone ML, Dobson BE, Mendelsohn C (2000). "Characteristics of patients with primary acute lateral patellar dislocation and their recovery within the first 6 months of injury". Am J Sports Med. 28 (4): 472–9. PMID 10921637.
- ↑ Ficat, R. Paul.; Hungerford, David S. (1977). Disorders of the patello-femoral join. Baltimore: Williams Wilkins. ISBN 0-683-03200-3.
- ↑ Zaffagnini, Stefano.; Dejour, David.; Arendt, Elizabeth A. (Elizabeth Anne) (2010). Patellofemoral pain, instabilty, and arthritis : clinical presentation, imaging, and treatmen. Heidelberg ; New York: Springer. ISBN 978-3-642-05423-5.
- ↑ Floyd, R. T. (2009). Manual of Structural Kinesiology. Boston: McGraw-Hill Higher Education. ISBN 978-0-07-337643-1.
- ↑ Dejour, H.; Walch, G.; Nove-Josserand, L.; Guier, C. (1994). "Factors of patellar instability: an anatomic radiographic study.". Knee Surg Sports Traumatol Arthrosc. 2 (1): 19–26. doi:10.1007/bf01552649. PMID 7584171.
- ↑ Saladin, Kenneth S. (2012). Anatomy & physiology : the unity of form and function (6th ed.). New York, NY: McGraw-Hill. p. 268. ISBN 978-0-07-337825-1.
- ↑ Family Practice Notebook > Patella Tracking Assessment by Scott Moses, last revised before 5/10/08
- ↑ Nomura, E.; Horiuchi, Y.; Kihara, M. (Apr 2000). "Medial patellofemoral ligament restraint in lateral patellar translation and reconstruction.". Knee. 7 (2): 121–127. doi:10.1016/s0968-0160(00)00038-7. PMID 10788776.
- ↑ Gerrard, DF. (May 1998). "External knee support in rugby union. Effectiveness of bracing and taping.". Sports Med. 25 (5): 313–7. doi:10.2165/00007256-199825050-00002. PMID 9629609.
- ↑ Abdulla, A. (Dec 2006). "Holiday review. Pills.". CMAJ. 175 (12): 1575. doi:10.1503/cmaj.061382. PMC 1660600
 . PMID 17146100.
. PMID 17146100. - 1 2 Waterman, BR.; Belmont, PJ.; Owens, BD. (Mar 2012). "Patellar dislocation in the United States: role of sex, age, race, and athletic participation.". J Knee Surg. 25 (1): 51–7. doi:10.1055/s-0031-1286199. PMID 22624248.
- ↑ Fithian, DC.; Paxton, EW.; Stone, ML.; Silva, P.; Davis, DK.; Elias, DA.; White, LM. (2004). "Epidemiology and natural history of acute patellar dislocation.". Am J Sports Med. 32 (5): 1114–21. doi:10.1177/0363546503260788. PMID 15262631.
- ↑ Sillanpää, Petri. "Treatment of Patellar Dislocation in Children" (PDF). patellofemoral.org. Patellofemoral Foundation.
- ↑ Palmu, Sauli; Kallio, Pentti E.; Donell, Simon T.; Helenius, Ilkka; Nietosvaara, Yrjänä (1 March 2008). "Acute Patellar Dislocation in Children and Adolescents: A Randomized Clinical Trial". The Journal of Bone & Joint Surgery. 90 (3): 463–470. doi:10.2106/JBJS.G.00072. ISSN 1535-1386. PMID 18310694.
Further reading
- The KNEEguru – educational site packed with knee content with sections on the patella
- University of Connecticut: New England Musculoskeletal Institute – site concerning knee injury treatment options