Methicillin-resistant Staphylococcus aureus
| Methicillin-resistant Staphylococcus aureus | |
|---|---|
 | |
| Scanning electron micrograph of a human neutrophil ingesting MRSA | |
| Scientific classification | |
| Domain: | Bacteria |
| Kingdom: | Eubacteria |
| Phylum: | Firmicutes |
| Class: | Bacilli |
| Order: | Bacillales |
| Family: | Staphylococcaceae |
| Genus: | Staphylococcus |
| Species: | S. aureus |
| Binomial name | |
| Staphylococcus aureus | |
Methicillin-resistant Staphylococcus aureus (MRSA) (/ɛmɑːrɛseɪ/ or /ˈmɜːrsə/) is a bacterium responsible for several difficult-to-treat infections in humans. MRSA is any strain of Staphylococcus aureus that has developed, through horizontal gene transfer and natural selection, multi- resistance to beta-lactam antibiotics, which include the penicillins (methicillin, dicloxacillin, nafcillin, oxacillin, etc.) and the cephalosporins. MRSA evolved from horizontal gene transfer of the mecA gene to at least five distinct S. aureus lineages.[1] Strains unable to resist these antibiotics are classified as methicillin-susceptible Staphylococcus aureus, or MSSA. The evolution of such resistance does not cause the organism to be more intrinsically virulent than strains of S. aureus that have no antibiotic resistance, but resistance does make MRSA infection more difficult to treat with standard types of antibiotics and thus more dangerous.
MRSA is especially troublesome in hospitals, prisons, and nursing homes, where patients with open wounds, invasive devices, and weakened immune systems are at greater risk of nosocomial infection (hospital-acquired infection) than the general public. MRSA began as a hospital-acquired infection, but has developed limited endemic status and is now sometimes community-acquired as well as livestock-acquired. The terms HA-MRSA (healthcare-associated MRSA), CA-MRSA (community-associated MRSA) and LA-MRSA (livestock-associated) reflect this distinction.
Signs and symptoms
S. aureus most commonly colonizes under the anterior nares (the nostrils).[2] The rest of the respiratory tract, open wounds, intravenous catheters, and the urinary tract are also potential sites for infection.[3] Healthy individuals may carry MRSA asymptomatically for periods ranging from a few weeks to many years. Patients with compromised immune systems are at a significantly greater risk of symptomatic secondary infection.
In most patients, MRSA can be detected by swabbing the nostrils and isolating the bacteria found inside the nostrils. Combined with extra sanitary measures for those in contact with infected patients, swab screening patients admitted to hospitals has been found to be effective in minimizing the spread of MRSA in hospitals in the United States,[4] Denmark, Finland, and the Netherlands.[5]
MRSA may progress substantially within 24–48 hours of initial topical symptoms.[3] After 72 hours, MRSA can take hold in human tissues and eventually become resistant to treatment. The initial presentation of MRSA is small red bumps that resemble pimples, spider bites, or boils; they may be accompanied by fever and, occasionally, rashes. Within a few days, the bumps become larger and more painful; they eventually open into deep, pus-filled boils.[6] About 75 percent of community-associated (CA-) MRSA infections are localized to skin and soft tissue and usually can be treated effectively.[7] Some CA-MRSA strains display enhanced virulence, spreading more rapidly and causing illness much more severe than traditional HA-MRSA infections, and they can affect vital organs and lead to widespread infection (sepsis), toxic shock syndrome, and necrotizing pneumonia. This is thought to be due to toxins carried by CA-MRSA strains, such as PVL and PSM, though PVL was recently found not to be a factor in a study by the National Institute of Allergy and Infectious Diseases at the National Institutes of Health. It is not known why some healthy people develop CA-MRSA skin infections that are treatable while others infected with the same strain develop severe infections or die.[8]
People are occasionally colonized with CA-MRSA and are completely asymptomatic. The most common manifestations of CA-MRSA are simple skin infections, such as impetigo, boils, abscesses, folliculitis, and cellulitis. Rarer, but more serious, manifestations can occur, such as necrotizing fasciitis and pyomyositis (most commonly found in the tropics), necrotizing pneumonia, and infective endocarditis (which affects the valves of the heart), and bone and joint infections.[9] CA-MRSA often results in abscess formation that requires incision and drainage. Before the spread of MRSA into the community, abscesses were not considered contagious, because infection was assumed to require violation of skin integrity and the introduction of staphylococci from normal skin colonization. However, newly emerging CA-MRSA is transmissible (similar, but with very important differences) from HA-MRSA. CA-MRSA is less likely than other forms of MRSA to cause cellulitis.
Risk factors
Some of the populations at risk:
- People who are frequently in crowded places, especially with shared equipment and skin-to-skin contact[10]
- People with weak immune systems (HIV/AIDS, lupus, or cancer sufferers; transplant recipients, severe asthmatics, etc.)
- Diabetics[11]
- Intravenous drug users[12][13]
- Users of quinolone antibiotics[14]
- The elderly[15]
- School children sharing sports and other equipment [3]
- College students living in dormitories[10]
- Women with frequent urinary tract or kidney infections due to infections in the bladder
- People staying or working in a health care facility for an extended period of time[10]
- People who spend time in coastal waters where MRSA is present, such as some beaches in Florida and the west coast of the United States[16][17]
- People who spend time in confined spaces with other people, including occupants of homeless shelters and warming centers, prison inmates, military recruits in basic training,[18] and individuals who spend considerable time in changing rooms or gyms
- Veterinarians, livestock handlers, and pet owners[19]
Hospital patients
Many MRSA infections occur in hospitals and healthcare facilities. Infections occurring in this manner are known as healthcare acquired MRSA (HA-MRSA). The rates of MRSA infection are also increased in hospitalized patients who are treated with quinolones. Healthcare provider-to-patient transfer is common, especially when healthcare providers move from patient to patient without performing necessary hand-washing techniques between patients.[14][20] Online tools predicting probability of nasal carriage in hospital admissions are available.[21]
Prison inmates, military recruits, and the homeless
Prisons, military barracks, and homeless shelters can be crowded and confined, and poor hygiene practices may proliferate, thus putting inhabitants at increased risk of contracting MRSA.[19] Cases of MRSA in such populations were first reported in the United States, and then in Canada. The earliest reports were made by the Center for Disease Control (CDC) in US state prisons. Subsequent reports of a massive rise in skin and soft tissue infections were reported by the CDC in the Los Angeles County Jail system in 2001, and this has continued. reported on the changing epidemiology of MRSA skin infection in the San Francisco County Jail, noting MRSA accounted for more than 70% of S. aureus infection in the jail by 2002. Lowy and colleagues reported on frequent MRSA skin infections in New York state prisons. Two reports on inmates in Maryland have demonstrated frequent colonization with MRSA.
In the news media, hundreds of reports of MRSA outbreaks in prisons appeared between 2000 and 2008. For example, in February 2008, the Tulsa County jail in Oklahoma started treating an average of 12 S. aureus cases per month.[22] A report on skin and soft tissue infections in the Cook County jail in Chicago in 2004–05 demonstrated MRSA was the most common cause of these infections among cultured lesions, and few risk factors were more strongly associated with MRSA infections than infections caused by methicillin-susceptible S. aureus. In response to these and many other reports on MRSA infections among incarcerated and recently incarcerated persons, the Federal Bureau of Prisons has released guidelines for the management and control of the infections, although few studies provide an evidence base for these guidelines.
Livestock
Cases of MRSA have increased in livestock animals. CC398, a new variant of MRSA, has emerged in animals and is found in intensively reared production animals (primarily pigs, but also cattle and poultry), where it can be transmitted to humans as LA-MRSA (livestock-associated MRSA). Though dangerous to humans, CC398 is often asymptomatic in food-producing animals.[23] In a single study conducted in Denmark, MRSA was shown to originate in livestock and spread to humans,[24] though the MRSA strain may have originated in humans and was transmitted to livestock.[25]
A 2011 study reported 47% of the meat and poultry sold in surveyed U.S. grocery stores was contaminated with S. aureus, and of those, 52% — or 24.4% of the total — were resistant to at least three classes of antibiotics. "Now we need to determine what this means in terms of risk to the consumer," said Dr. Keim, a co-author of the paper.[26] Some samples of commercially sold meat products in Japan were also found to harbor MRSA strains.[27]
An investigation of 100 pork samples purchased from major UK retailers conducted by the Guardian in 2015 showed that some 10% of the samples were contaminated.[28]
Athletes
Locker rooms, gyms, and related athletic facilities offer potential sites for MRSA contamination and infection.[29] A study linked MRSA to the abrasions caused by artificial turf.[30] Three studies by the Texas State Department of Health found the infection rate among football players was 16 times the national average. In October 2006, a high-school football player was temporarily paralyzed from MRSA-infected turf burns. His infection returned in January 2007 and required three surgeries to remove infected tissue, as well as three weeks of hospital stay.[31] In 2013, Lawrence Tynes, Carl Nicks, and Johnthan Banks of the Tampa Bay Buccaneers were diagnosed with MRSA. Tynes and Nicks apparently did not contract the infection from each other, but it is unknown if Banks contracted it from either individual.[32] In 2015, Los Angeles Dodgers' infielder Justin Turner was infected while the team visited the New York Mets.[33] In October 2015, New York Giants tight end Daniel Fells was hospitalized with a serious MRSA infection.[34]
Children
MRSA is becoming a critical problem in pediatric settings;[35] recent studies found 4.6% of patients in U.S. health-care facilities, (presumably) including hospital nurseries,[36] were infected or colonized with MRSA.[37] Children (and adults, as well) who come in contact with day-care centers, playgrounds, locker rooms, camps, dormitories, classrooms and other school settings, and gyms and workout facilities are at higher risk of getting MRSA. Parents should be especially cautious of children who participate in activities where sports equipment is shared, such as football helmets and uniforms.[38]
Diagnosis


Diagnostic microbiology laboratories and reference laboratories are key for identifying outbreaks of MRSA. Faster techniques for identifying and characterizing MRSA have recently been developed.[39] Normally, the bacterium must be cultured from blood, urine, sputum, or other body-fluid samples, and in sufficient quantities to perform confirmatory tests early-on. Still, because no quick and easy method exists to diagnose MRSA, initial treatment of the infection is often based upon 'strong suspicion' and techniques by the treating physician; these include quantitative PCR procedures, which are employed in clinical laboratories for quickly detecting and identifying MRSA strains.[40][41]
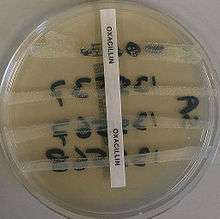
Another common laboratory test is a rapid latex agglutination test that detects the PBP2a protein. PBP2a is a variant penicillin-binding protein that imparts the ability of S. aureus to be resistant to oxacillin.[42]
Genetics
Antimicrobial resistance is genetically based; resistance is mediated by the acquisition of extrachromosomal genetic elements containing resistance genes. Examples include plasmids, transposable genetic elements, and genomic islands, which are transferred between bacteria through horizontal gene transfer.[43] A defining characteristic of MRSA is its ability to thrive in the presence of penicillin-like antibiotics, which normally prevent bacterial growth by inhibiting synthesis of cell wall material. This is due to a resistance gene, mecA, which stops β-lactam antibiotics from inactivating the enzymes (transpeptidases) critical for cell wall synthesis.
SCCmec
Staphylococcal cassette chromosome mec (SCCmec) is a genomic island of unknown origin containing the antibiotic resistance gene mecA.[44][45] SCCmec contains additional genes beyond mecA, including the cytolysin gene psm-mec, which may suppress virulence in HA-acquired MRSA strains.[46] SCCmec also contains ccrA and ccrB; both genes encode recombinases that mediate the site-specific integration and excision of the SCCmec element from the S. aureus chromosome.[44][45] Currently, six unique SCCmec types ranging in size from 21–67 kb have been identified;[44] they are designated types I-VI and are distinguished by variation in mec and ccr gene complexes.[43] Owing to the size of the SCCmec element and the constraints of horizontal gene transfer, a minimum of five clones are thought to be responsible for the spread of MRSA infections, with clonal complex (CC) 8 most prevalent.[44][47] SCCmec is thought to have originated in the closely related Staphylococcus sciuri species and transferred horizontally to S. aureus. [48]
Different SCCmec genotypes confer different microbiological characteristics, such as different antimicrobial resistance rates.[49] Different genotypes are also associated with different types of infections. Types I-III SCCmec are large elements that typically contain additional resistance genes and are characteristically isolated from HA-MRSA strains.[45][49] Conversely, CA-MRSA is associated with types IV and V, which are smaller and lack resistance genes other than mecA.[45][49]
These distinctions were thoroughly investigated by Collins et al. in 2001 and can be explained by the fitness differences associated with carriage of a large or small SCCmec plasmid. Carriage of large plasmids, such as SCCmecI-III, is costly to the bacteria, resulting in compensatory decrease in virulence expression.[50] MRSA is able to thrive in hospital settings with increased antibiotic resistance but decreased virulence- HA-MRSA targets immunocompromised, hospitalized hosts, thus a decrease in virulence is not maladaptive.[50] In contrast, CA-MRSA tends to carry lower fitness cost SCCmec elements to offset the increased virulence and toxicity expression required to infect healthy hosts.[50]
mecA
mecA is a biomarker gene responsible for resistance to methicillin and other β-lactam antibiotics.[3] After acquisition of mecA, the gene must be integrated and localized in the S. aureus chromosome.[44] mecA encodes penicillin-binding protein 2a (PBP2a), which differs from other penicillin-binding proteins as its active site does not bind methicillin or other β-lactam antibiotics.[44] As such, PBP2a can continue to catalyze the transpeptidation reaction required for peptidoglycan cross-linking, enabling cell wall synthesis in the presence of antibiotics. As a consequence of the inability of PBP2a to interact with β-lactam moieties, acquisition of mecA confers resistance to all β-lactam antibiotics in addition to methicillin.[44][51]
mecA is under the control of two regulatory genes, mecI and mecR1. MecI is usually bound to the mecA promoter and functions as a repressor.[43][45] In the presence of a β-lactam antibiotic, MecR1 initiates a signal transduction cascade that leads to transcriptional activation of mecA.[43][45] This is achieved by MecR1-mediated cleavage of MecI, which alleviates MecI repression.[43] mecA is further controlled by two co-repressors, BlaI and BlaR1. blaI and blaR1 are homologous to mecI and mecR1, respectively, and normally function as regulators of blaZ, which is responsible for penicillin resistance.[44][52] The DNA sequences bound by MecI and BlaI are identical;[44] therefore, BlaI can also bind the mecA operator to repress transcription of mecA.[52]
Arginine catabolic mobile element
The arginine catabolic mobile element (ACME) is a virulence factor present in many MRSA strains but not prevalent in MSSA.[53] SpeG-positive ACME compensates for the polyamine hypersensitivity of S. aureus and facilitates stable skin colonization, wound infection, and person-to-person transmission.
Strains

Acquisition of SCCmec in methicillin-sensitive staphylococcus aureus (MSSA) gives rise to a number of genetically different MRSA lineages. These genetic variations within different MRSA strains possibly explain the variability in virulence and associated MRSA infections.[54] The first MRSA strain, ST250 MRSA-1 originated from SCCmec and ST250-MSSA integration.[54] Historically, major MRSA clones: ST2470-MRSA-I, ST239-MRSA-III, ST5-MRSA-II, and ST5-MRSA-IV were responsible for causing hospital-acquired MRSA (HA-MRSA) infections.[54] ST239-MRSA-III, known as the Brazilian clone, was highly transmissible compared to others and distributed in Argentina, Czech Republic, and Portugal.[54]
In the UK, the most common strains of MRSA are EMRSA15 and EMRSA16.[55] EMRSA16 is the best described epidemiologically: it originated in Kettering, England, and the full genomic sequence of this strain has been published.[56] EMRSA16 has been found to be identical to the ST36:USA200 strain, which circulates in the United States, and to carry the SCCmec type II, enterotoxin A and toxic shock syndrome toxin 1 genes.[57] Under the new international typing system, this strain is now called MRSA252. EMRSA 15 is also found to be one of the common MRSA strains in Asia. Other common strains include ST5:USA100 and EMRSA 1.[58] These strains are genetic characteristics of HA-MRSA.[59]
It is not entirely certain why some strains are highly transmissible and persistent in healthcare facilities.[54] One explanation is the characteristic pattern of antibiotic susceptibility. Both the EMRSA15 and EMRSA16 strains are resistant to erythromycin and ciprofloxacin. It is known that Staphylococcus aureus can survive intracellularly,[60] for example in the nasal mucosa [61] and in the tonsil tissue.[62] Erythromycin and ciprofloxacin are precisely the antibiotics that best penetrate intracellularly; it may be that these strains of S. aureus are therefore able to exploit an intracellular niche.
Community-acquired MRSA (CA-MRSA) strains emerged in late 1990 to 2000, infecting healthy people who had not been in contact with health care facilities.[59] A later study that analyzed data from more than 300 microbiology labs associated with hospitals all over the United States have found a seven-fold increase, jumping from 3.6% of all MRSA infections to 28.2%, in the proportion of community-associated strains of MRSA between 1999 and 2006.[63] Researchers suggest that CA-MRSA did not evolve from the HA-MRSA.[59] This is further proven by molecular typing of CA-MRSA strains[64] and genome comparison between CA-MRSA and HA-MRSA, which indicate that novel MRSA strains integrated SCCmec into MSSA separately on its own.[59] By mid 2000, CA-MRSA was introduced into the health care systems and distinguishing CA-MRSA from HA-MRSA became a difficult process.[59] Community-acquired MRSA (CA-MRSA) is more easily treated and more virulent than hospital-acquired MRSA (HA-MRSA).[59] The genetic mechanism for the enhanced virulence in CA-MRSA remains an active area of research. Especially the Panton–Valentine leukocidin (PVL) genes are of interest because they are a unique feature of CA-MRSA.[54]
In the United States, most cases of CA-MRSA are caused by a CC8 strain designated ST8:USA300, which carries SCCmec type IV, Panton–Valentine leukocidin, PSM-alpha and enterotoxins Q and K,[57] and ST1:USA400.[65] The ST8:USA300 strain results in skin infections, necrotizing fasciitis and toxic shock syndrome, whereas the ST1:USA400 strain results in necrotizing pneumonia and pulmonary sepsis.[54] Other community-acquired strains of MRSA are ST8:USA500 and ST59:USA1000. In many nations of the world, MRSA strains with different predominant genetic background types have come to predominate among CA-MRSA strains; USA300 easily tops the list in the U.S. and is becoming more common in Canada after its first appearance there in 2004. For example, in Australia ST93 strains are common, while in continental Europe ST80 strains, which carry SCCmec type IV, predominate.[66][67] In Taiwan, ST59 strains, some of which are resistant to many non-beta-lactam antibiotics, have arisen as common causes of skin and soft tissue infections in the community. In a remote region of Alaska, unlike most of the continental U.S., USA300 was found rarely in a study of MRSA strains from outbreaks in 1996 and 2000 as well as in surveillance from 2004–06.[68] In 2015, CA-MRSA has been reported in the urban and rural school settings of Kurdistan, Iraq.[3]
In June 2011, the discovery of a new strain of MRSA was announced by two separate teams of researchers in the UK. Its genetic makeup was reportedly more similar to strains found in animals, and testing kits designed to detect MRSA were unable to identify it.[69] This MRSA strain, Clonal Complex 398 (CC398), is responsible for Livestock-associated MRSA (LA-MRSA) infections.[58] Although it is known to be more persistent in colonizing pigs and calves, there have been cases of LA-MRSA carriers with pneumonia, endocarditis, and necrotising fasciitis.[70]
Prevention
Screening programs
Patient screening upon hospital admission, with nasal cultures, prevents the cohabitation of MRSA carriers with non-carriers, and exposure to infected surfaces. The test used (whether a rapid molecular method or traditional culture) is not as important as the implementation of active screening.[71] In the United States and Canada, the Centers for Disease Control and Prevention issued guidelines on October 19, 2006, citing the need for additional research, but declined to recommend such screening.[72][73]
In some UK hospitals screening for MRSA is performed in every patient[74] and all NHS surgical patients, except for minor surgeries, are previously checked for MRSA.[75] There is no community screening in the UK; however, screening of individuals is offered by some private companies.[76]
In a US cohort of 1300 healthy children, 2.4% carried MRSA in their nose.[77]
Surface sanitizing

Alcohol has been proven to be an effective surface sanitizer against MRSA. Quaternary ammonium compounds can be used in conjunction with alcohol to extend the longevity of the sanitizing action. The prevention of nosocomial infections involves routine and terminal cleaning. Non-flammable alcohol vapor in carbon dioxide systems (NAV-CO2) do not corrode metals or plastics used in medical environments and do not contribute to antibacterial resistance.
In healthcare environments, MRSA can survive on surfaces and fabrics, including privacy curtains or garments worn by care providers. Complete surface sanitation is necessary to eliminate MRSA in areas where patients are recovering from invasive procedures. Testing patients for MRSA upon admission, isolating MRSA-positive patients, decolonization of MRSA-positive patients, and terminal cleaning of patients' rooms and all other clinical areas they occupy is the current best practice protocol for nosocomial MRSA.
Studies published from 2004-2007 reported hydrogen peroxide vapor could be used to decontaminate busy hospital rooms, despite taking significantly longer than traditional cleaning. One study noted rapid recontamination by MRSA following the hydrogen peroxide application.[78][79][80][81][82]
Also tested, in 2006, was a new type of surface cleaner, incorporating accelerated hydrogen peroxide, which was pronounced "a potential candidate" for use against the targeted microorganisms.[83]
Research on copper alloys
In 2008, after evaluating a wide body of research mandated specifically by the United States Environmental Protection Agency (EPA), registration approvals were granted by EPA in 2008 granting that copper alloys kill more than 99.9% of MRSA within two hours.
Subsequent research conducted at the University of Southampton (UK) compared the antimicrobial efficacies of copper and several non-copper proprietary coating products to kill MRSA.[84][85] At 20 °C, the drop-off in MRSA organisms on copper alloy C11000 is dramatic and almost complete (over 99.9% kill rate) within 75 minutes. However, neither a triclosan-based product nor two silver-containing based antimicrobial treatments (Ag-A and Ag-B) exhibited any meaningful efficacy against MRSA. Stainless steel S30400 did not exhibit any antimicrobial efficacy.
In 2004, the University of Southampton research team was the first to clearly demonstrate that copper inhibits MRSA.[86] On copper alloys — C19700 (99% copper), C24000 (80% copper), and C77000 (55% copper) — significant reductions in viability were achieved at room temperatures after 1.5 hours, 3.0 hours and 4.5 hours, respectively. Faster antimicrobial efficacies were associated with higher copper alloy content. Stainless steel did not exhibit any bactericidal benefits.
Hand washing
In September 2004,[87] after a successful pilot scheme to tackle MRSA, the UK National Health Service announced its Clean Your Hands campaign. Wards were required to ensure that alcohol-based hand rubs are placed near all beds so that staff can hand wash more regularly. It is thought that even if this cuts infection by no more than 1%, the plan will pay for itself many times over.
As with some other bacteria, MRSA is acquiring more resistance to some disinfectants and antiseptics. Although alcohol-based rubs remain somewhat effective, a more effective strategy is to wash hands with running water and an antimicrobial cleanser with persistent killing action, such as chlorhexidine.[88] In another study chlorhexidine (Hibiclens), p-chloro-m-xylenol (Acute-Kare), hexachlorophene (Phisohex), and povidone-iodine (Betadine) were evaluated for their effectiveness. Of the four most commonly used antiseptics, povidone-iodine, when diluted 1:100, was the most rapidly bactericidal against both MRSA and methicillin-susceptible S. aureus.[89]
A June 2008 report, centered on a survey by the Association for Professionals in Infection Control and Epidemiology, concluded that poor hygiene habits remain the principal barrier to significant reductions in the spread of MRSA.
Proper disposal of hospital gowns
Used paper hospital gowns are associated with MRSA hospital infections, which could be avoided by proper disposal.[90]
Isolation
Excluding medical facilities, current US guidance does not require workers with MRSA infections to be routinely excluded from the general workplace.[91] Therefore, unless directed by a health care provider, exclusion from work should be reserved for those with wound drainage that cannot be covered and contained with a clean, dry bandage and for those who cannot maintain good hygiene practices.[91] Workers with active infections should be excluded from activities where skin-to-skin contact is likely to occur until their infections are healed. Health care workers should follow the Centers for Disease Control and Prevention's Guidelines for Infection Control in Health Care Personnel.[92]
To prevent the spread of staph or MRSA in the workplace, employers should ensure the availability of adequate facilities and supplies that encourage workers to practice good hygiene; that surface sanitizing in the workplace is followed; and that contaminated equipment are sanitized with Environmental Protection Agency (EPA)-registered disinfectants.[91]
Restricting antibiotic use
Glycopeptides, cephalosporins, and, in particular, quinolones are associated with an increased risk of colonisation of MRSA. Reducing use of antibiotic classes that promote MRSA colonisation, especially fluoroquinolones, is recommended in current guidelines.[14][20]
Public health considerations
The burden of MRSA is significant. In 2009, there were an estimated 463,017 (95% confidence interval: 441,595, 484,439) MRSA-related hospitalizations, or a rate of 11.74 (95% confidence interval: 11.20, 12.28) per 1,000 hospitalizations.[93] Many of these infections are less serious, but the Centers for Disease Control and Prevention (CDC) estimates that there are 80,461 invasive MRSA infections and 11,285 deaths due to MRSA annually.[94]
Mathematical models describe one way in which a loss of infection control can occur after measures for screening and isolation seem to be effective for years, as happened in the UK. In the "search and destroy" strategy that was employed by all UK hospitals until the mid-1990s, all patients with MRSA were immediately isolated, and all staff were screened for MRSA and were prevented from working until they had completed a course of eradication therapy that was proven to work. Loss of control occurs because colonised patients are discharged back into the community and then readmitted; when the number of colonised patients in the community reaches a certain threshold, the "search and destroy" strategy is overwhelmed.[95] One of the few countries not to have been overwhelmed by MRSA is the Netherlands: An important part of the success of the Dutch strategy may have been to attempt eradication of carriage upon discharge from hospital.[96]
The Centers for Disease Control and Prevention (CDC) estimated that about 1.7 million nosocomial infections occurred in the United States in 2002, with 99,000 associated deaths.[97] The estimated incidence is 4.5 nosocomial infections per 100 admissions, with direct costs (at 2004 prices) ranging from $10,500 (£5300, €8000 at 2006 rates) per case (for bloodstream, urinary tract, or respiratory infections in immunocompetent patients) to $111,000 (£57,000, €85,000) per case for antibiotic-resistant infections in the bloodstream in patients with transplants. With these numbers, conservative estimates of the total direct costs of nosocomial infections are above $17 billion. The reduction of such infections forms an important component of efforts to improve healthcare safety. (BMJ 2007) MRSA alone was associated with 8% of nosocomial infections reported to the CDC National Healthcare Safety Network from January 2006 to October 2007.[98]
This problem is not unique to one country; the British National Audit Office estimated that the incidence of nosocomial infections in Europe ranges from 4% to 10% of all hospital admissions. As of early 2005, the number of deaths in the United Kingdom attributed to MRSA has been estimated by various sources to lie in the area of 3,000 per year.[99] Staphylococcus bacteria account for almost half of all UK hospital infections. The issue of MRSA infections in hospitals has recently been a major political issue in the UK, playing a significant role in the debates over health policy in the United Kingdom general election held in 2005.
On January 6, 2008, half of 64 non-Chinese cases of MRSA infections in Hong Kong in 2007 were Filipino domestic helpers. Ho Pak-leung, professor of microbiology at the University of Hong Kong, traced the cause to high use of antibiotics. In 2007, there were 166 community cases in Hong Kong compared with 8,000 hospital-acquired MRSA cases (155 recorded cases—91 involved Chinese locals, 33 Filipinos, 5 each for Americans and Indians, and 2 each from Nepal, Australia, Denmark and England).[100]
Worldwide, an estimated 2 billion people carry some form of S. aureus; of these, up to 53 million (2.7% of carriers) are thought to carry MRSA.[101] In the United States, 95 million carry S. aureus in their noses; of these, 2.5 million (2.6% of carriers) carry MRSA.[102] A population review conducted in three U.S. communities showed the annual incidence of CA-MRSA during 2001–2002 to be 18–25.7/100,000; most CA-MRSA isolates were associated with clinically relevant infections, and 23% of patients required hospitalization.[103]
One possible contribution to the increased spread of MRSA infections comes from the use of antibiotics in intensive pig farming. A 2008 study in Canada found MRSA in 10% of tested pork chops and ground pork; a U.S. study in the same year found MRSA in the noses of 70% of the tested farm pigs and in 45% of the tested pig farm workers.[104] There have also been anecdotal reports of increased MRSA infection rates in rural communities with pig farms.[105]
Healthcare facilities with high bed occupancy rates, high levels of temporary nursing staff, or low cleanliness scores no longer have significantly higher MRSA rates. Simple tabular evidence helps provide a clear picture of these changes, showing, for instance, that hospitals with occupancy over 90% had, in 2006–2007, MRSA rates little above those in hospitals with occupancy below 85%, in contrast to the period 2001–2004. In one sense, the disappearance of these relationships is puzzling. Reporters now blame IV cannula and catheters for spreading MRSA in hospitals. (Hospital organisation and speciality mix, 2008)
Decolonization
Care should be taken when trying to drain boils, as disruption of surrounding tissue can lead to larger infections, or even infection of the blood stream (often with fatal consequences).[106] Any drainage should be disposed of very carefully. After the drainage of boils or other treatment for MRSA, patients can shower at home using chlorhexidine (Hibiclens) or hexachlorophene (Phisohex) antiseptic soap (available over-the-counter at many pharmacies) from head to toe. Alternatively, a dilute bleach bath can be taken at a concentration of 2.5 μL/mL dilution of bleach (about 1/2 cup bleach per 1/4-full bathtub of water).[107] Care should be taken to use a clean towel, and to ensure that nasal discharge doesn't infect the towel (see below).
All infectious lesions should be kept covered with a dressing.[106] Mupirocin (Bactroban) 2% ointment can be effective at reducing the size of lesions. A secondary covering of clothing is preferred.[108] As shown in an animal study with diabetic mice, the topical application of a mixture of sugar (70%) and 3% povidone-iodine paste is an effective agent for the treatment of diabetic ulcers with MRSA infection.[109]
The nose is a common refuge for MRSA, and a test swab can be taken of the nose to indicate whether MRSA is present.[110] If MRSA is detected via nasal culture, Mupirocin (Bactroban) 2% ointment can be applied inside each nostril twice daily for 7 days, using a cotton-tipped swab. However, care should be taken so that the swab doesn't penetrate into the sinus. Household members are recommended to follow the same decolonization protocol. After treatment, the nose should be swabbed again to ensure that the treatment was effective. If not, the process should be repeated.
In the hospital setting toilet seats are a common vector for infection, and wiping seats clean before and/or after use can help to prevent the spread of MRSA. Door handles, faucets, light switches, etc. can be disinfected regularly with disinfectant wipes.[108] Spray disinfectants can be used on upholstery. Carpets can be washed with disinfectant, and hardwood floors can be scrubbed with diluted tea tree oil (e.g. Melaleuca). Laundry soap containing tea tree oil may be effective at decontaminating clothing and bedding, especially if hot water and heavy soil cycles are used, however tea tree oil may cause a rash which MRSA can re-colonize. Alcohol-based sanitizers can be placed near bedsides, near sitting areas, in vehicles etc. to encourage their use.
Doctors may also prescribe antibiotics such as clindamycin, doxycycline, or trimethoprim/sulfamethoxazole.
Community settings
The CDC offers suggestions for preventing the contraction and spread MRSA infection which are applicable to those in community settings, including incarcerated populations, childcare center employees, and athletes. To prevent MRSA infection, individuals should regularly wash hands using soap and water or an alcohol-based sanitizer, keep wounds clean and covered, avoid contact with other people's wounds, avoid sharing personal items such as razors or towels, shower after exercising at athletic facilities (including gyms, weight rooms, and school facilities), shower before using swimming pools or whirlpools, and maintain a clean environment.[111]
It may be difficult for people to maintain the necessary cleanliness if they do not have access to facilities such as public toilets with handwashing facilities. In the United Kingdom, the Workplace (Health, Safety and Welfare) Regulations 1992 requires businesses to provide toilets for their employees, along with washing facilities including soap or other suitable means of cleaning. Guidance on how many toilets to provide and what sort of washing facilities should be provided alongside them is given in the Workplace (Health, Safety and Welfare) Approved Code of Practice and Guidance L24, available from Health and Safety Executive Books. But there is no legal obligation on local authorities in the United Kingdom to provide public toilets, and although in 2008 the House of Commons Communities and Local Government Committee called for a duty on local authorities to develop a public toilet strategy[112] this was rejected by the Government.[113]
Treatment
Both CA-MRSA and HA-MRSA are resistant to traditional anti-staphylococcal beta-lactam antibiotics, such as cephalexin. CA-MRSA has a greater spectrum of antimicrobial susceptibility, including to sulfa drugs (like co-trimoxazole (trimethoprim/sulfamethoxazole)), tetracyclines (like doxycycline and minocycline) and clindamycin (for osteomyelitis), but the drug of choice for treating CA-MRSA is now believed to be vancomycin, according to a Henry Ford Hospital Study. HA-MRSA is resistant even to these antibiotics and often is susceptible only to vancomycin. Newer drugs, such as linezolid (belonging to the newer oxazolidinones class) and daptomycin, are effective against both CA-MRSA and HA-MRSA. The Infectious Disease Society of America recommends vancomycin, linezolid, or clindamycin (if susceptible) for treating patients with MRSA pneumonia.[114] Ceftaroline, a fifth-generation cephalosporin, is the first beta-lactam antibiotic approved in the US to treat MRSA infections (skin and soft tissue or community acquired pneumonia only).[115]
Vancomycin and teicoplanin are glycopeptide antibiotics used to treat MRSA infections.[116] Teicoplanin is a structural congener of vancomycin that has a similar activity spectrum but a longer half-life.[117] Because the oral absorption of vancomycin and teicoplanin is very low, these agents must be administered intravenously to control systemic infections.[118] Treatment of MRSA infection with vancomycin can be complicated, due to its inconvenient route of administration. Moreover, many clinicians believe that the efficacy of vancomycin against MRSA is inferior to that of anti-staphylococcal beta-lactam antibiotics against methicillin-susceptible Staphylococcus aureus (MSSA).[119][120]
Several newly discovered strains of MRSA show antibiotic resistance even to vancomycin and teicoplanin. These new evolutions of the MRSA bacterium have been dubbed vancomycin intermediate-resistant Staphylococcus aureus (VISA).[121] [122] Linezolid, quinupristin/dalfopristin, daptomycin, ceftaroline, and tigecycline are used to treat more severe infections that do not respond to glycopeptides such as vancomycin.[123] Current guidelines recommend daptomycin for VISA bloodstream infections and endocarditis.[124]
History
United States and United Kingdom

In 1959 methicillin was licensed in England to treat penicillin-resistant S. aureus infections. Just as bacterial evolution had allowed microbes to develop resistance to penicillin, strains of S. aureus evolved to become resistant to methicillin. In 1961 the first known MRSA isolates were reported in a British study, and from 1961 to 1967 there were infrequent hospital outbreaks in Western Europe and Australia.[125] The first United States hospital outbreak of MRSA occurred at the Boston City Hospital in 1968. From 1968 to the mid-1990s the percent of S. aureus infections that were caused by MRSA increased steadily, and MRSA became recognized as an endemic pathogen. In 1974 2% of hospital-acquired S. aureus infections could be attributed to MRSA.[126] The rate had increased to 22% by 1995, and by 1997 the percent of hospital S. aureus infections attributable to MRSA had reached 50%.
The first report of CA-MRSA occurred in 1981, and in 1982 there was a large outbreak of CA-MRSA among intravenous drug users in Detroit, Michigan.[125] Additional outbreaks of CA-MRSA were reported through the 1980s and 1990s, including outbreaks among Australian Aboriginal populations that had never been exposed to hospitals. In the mid-1990s there were scattered reports of CA-MRSA outbreaks among US children. While HA-MRSA rates stabilized between 1998 and 2008, CA-MRSA rates continued to rise. A report released by the University of Chicago Children's Hospital comparing two time periods (1993–1995 and 1995–1997) found a 25-fold increase in the rate of hospitalizations due to MRSA among children in the United States.[127] In 1999 the University of Chicago reported the first deaths from invasive MRSA among otherwise healthy children in the United States.[125] By 2004 MRSA accounted for 64% of hospital-acquired S. aureus infections in the United States.
The Office for National Statistics reported 1,629 MRSA-related deaths in England and Wales during 2005, indicating a MRSA-related mortality rate half the rate of that in the United States for 2005, even though the figures from the British source were explained to be high because of "improved levels of reporting, possibly brought about by the continued high public profile of the disease"[128] during the time of the 2005 United Kingdom General Election. MRSA is thought to have caused 1,652 deaths in 2006 in UK up from 51 in 1993.[129]
It has been argued that the observed increased mortality among MRSA-infected patients may be the result of the increased underlying morbidity of these patients. Several studies, however, including one by Blot and colleagues, that have adjusted for underlying disease still found MRSA bacteremia to have a higher attributable mortality than methicillin-susceptible S. aureus (MSSA) bacteremia.[130]
A population-based study of the incidence of MRSA infections in San Francisco during 2004–05 demonstrated that nearly 1 in 300 residents suffered from such an infection in the course of a year and that greater than 85% of these infections occurred outside of the healthcare setting.[131] A 2004 study showed that patients in the United States with S. aureus infection had, on average, three times the length of hospital stay (14.3 vs. 4.5 days), incurred three times the total cost ($48,824 vs. $14,141), and experienced five times the risk of in-hospital death (11.2% vs 2.3%) than patients without this infection.[132] In a meta-analysis of 31 studies, Cosgrove et al.,[133] concluded that MRSA bacteremia is associated with increased mortality as compared with MSSA bacteremia (odds ratio= 1.93; 95% CI = 1.93 ± 0.39).[134] In addition, Wyllie et al. report a death rate of 34% within 30 days among patients infected with MRSA, a rate similar to the death rate of 27% seen among MSSA-infected patients.[135]
According to the CDC, the most recent estimates of the incidence of healthcare-associated infections that are attributable to MRSA in the United States indicate a decline in such infection rates. Incidence of MRSA central line-associated blood stream infections as reported by hundreds of intensive care units decreased 50–70% from 2001–2007.[126] A separate system tracking all hospital MRSA bloodstream infections found an overall 34% decrease between 2005–2008.[126]
MRSA is sometimes sub-categorised as community-acquired MRSA (CA-MRSA) or healthcare-associated MRSA (HA-MRSA), although the distinction is complex. Some researchers have defined CA-MRSA by the characteristics of patients whom it infects, while others define it by the genetic characteristics of the bacteria. By 2005, identified CA-MRSA risk factors included athletes, military recruits, incarcerated people, emergency room patients, urban children, HIV-positive individuals, men who have sex with men, and indigenous populations.[125]
By 2015 the proportion of resistant infections in the UK had dropped from 40% down to about 15% a result of intense efforts in hospital hygiene.[136]
Worldwide
The first reported cases of CA-MRSA began to appear in the mid-1990s in Australia, New Zealand, the United States, the United Kingdom, France, Finland, Canada and Samoa, and were notable because they involved people who had not been exposed to a healthcare setting.[9]
Because measurement and reporting varies, it is difficult to compare rates of MRSA in different countries. An international comparison of 2004 MRSA-attributable S. aureus rates in middle and high income countries released by the Center For Disease Dynamics, Economics, and Policy in showed that Iceland had the lowest rate of infection, and Romania had the highest at over 70%.[137]
Across Europe, based mostly on data from 2013 seven countries (Iceland, Norway, Sweden, Netherlands, Denmark, Finland, and Estonia, from lowest to higher) had low levels of hospital-acquired MRSA infections compared to the others,[138]:92–93 and among countries with higher levels significant improvements had been made only in Bulgaria, Poland and the British Isles.[138]:40
Research
Clinical
Many antibiotics against MRSA are in phase II and phase III clinical trials. e.g.:
- Phase III: ceftobiprole, ceftaroline, dalbavancin, telavancin, torezolid, iclaprim, and others.
- Phase II: nemonoxacin.[139]
Development of Aurograb, a treatment intended to complement antibiotics used to treat MRSA, was discontinued after showing a lack of efficacy in Phase II trials.[140]
It has been reported that maggot therapy to clean out necrotic tissue of MRSA infection has been successful. Studies in diabetic patients reported significantly shorter treatment times than those achieved with standard treatments.[141][142][143]
Pre-clinical
Phage therapy
An entirely different approach is phage therapy (e.g., at the George Eliava Institute in Georgia[144]). Experimental phage therapy tested in mice had a reported efficacy against up to 95% of tested Staphylococcus isolates.[145]
Antibiotics
- On May 18, 2006, a report in Nature identified a new antibiotic, called platensimycin, that had demonstrated successful use against MRSA.[146][147]
- A new class of non-β-lactam antibiotics, oxadiazoles, was reported to be effective against MRSA infection in mouse models. The mechanisms of oxadiazoles’ antibacterial effect are the inhibition of the penicillin binding protein, PBP2a and biosynthesis of the bacterial cell wall. It was found to have bactericidal activity against vancomycin- and linezolid-resistant MRSA and other Gram-positive bacterial strains.[148][149]
Other treatments
- Some in vitro studies with honey have identified components in honey that kill MRSA.[150][151]
- Ocean-dwelling living sponges produce compounds that may make MRSA more susceptible to antibiotics.[152]
- Some semi-toxic fungi/mushrooms excrete broad-spectrum antibiotics, not all of which have been fully identified; some have been shown to inhibit the growth of Staphylococcus aureus.[153]
- An in vitro study showed that the cannabinoids CBD and CBG inhibit MRSA,[154] in addition to the terpenoid pinene which occurs in cannabis.[155]
- Cannabinoids (components of Cannabis sativa), including cannabidiol (CBD), cannabinol (CBN), cannabichromene (CBC), tetrahydrocannabinol (THC), and cannabigerol (CBG), show activity against a variety of MRSA strains.[156]
- In vitro studies have shown that oakin, an oak extract, can kill MRSA.[157]
- A 1,000-year-old eye salve recipe found in the medieval Bald's Leechbook at the British Library, one of the earliest known medical textbooks, was found to have activity against MRSA in vitro and in skin wounds in mice.[158]
- Some studies suggest that allicin, a compound found in garlic, may prove to be effective in the treatment of MRSA.[159]
Additional images
| Wikimedia Commons has media related to MRSA. |
 A colourised SEM of MRSA
A colourised SEM of MRSA Scanning electron micrograph of a human neutrophil ingesting MRSA
Scanning electron micrograph of a human neutrophil ingesting MRSA Scanning electron micrograph of a human neutrophil ingesting MRSA
Scanning electron micrograph of a human neutrophil ingesting MRSA_Bacteria.jpg) Scanning electron micrograph of a human neutrophil ingesting MRSA
Scanning electron micrograph of a human neutrophil ingesting MRSA
See also
- Carbapenem resistant enterobacteriaceae
- Necrotizing fasciitis
- Staphylococcus aureus
- Teixobactin
- Toxic shock syndrome
- XF-73
References
- ↑ Fitzgerald, J.R.; Sturdevant, D.E. (2001). "Evolutionary genomics of Staphylococcus aureus: Insights into the origin of methicillin-resistant strains and the toxic shock syndrome epidemic". PNAS. 98.
- ↑ Yan M, Pamp SJ, Fukuyama J, Hwang PH, Cho DY, Holmes S, Relman DA (2013). "Nasal microenvironments and interspecific interactions influence nasal microbiota complexity and S. aureus carriage". Cell Host Microbe. 14 (6): 631–40. doi:10.1016/j.chom.2013.11.005. PMC 3902146
 . PMID 24331461.
. PMID 24331461. - 1 2 3 4 5 Hussein, N. R.; Basharat, Z.; Muhammed, A. H.; Al-Dabbagh, S. A. (2015). "Comparative Evaluation of MRSA Nasal Colonization Epidemiology in the Urban and Rural Secondary School Community of Kurdistan, Iraq". PLOS ONE. 10 (5): e0124920. doi:10.1371/journal.pone.0124920. ISSN 1932-6203. PMC 4416827
 . PMID 25932644.
. PMID 25932644. - ↑ Lamfon, Medhat, A., PhD (7 April 2013). "The Control and Prevention of Methicillin Resistant Staphylococcus Aureus". The World Scientists. Archived from the original on 13 August 2016. Retrieved 13 August 2016.
- ↑ McCaughey B. "Unnecessary Deaths: The Human and Financial Costs of Hospital Infections" (PDF) (2nd ed.). Archived from the original (PDF) on July 11, 2007. Retrieved 2007-08-05.
- ↑ "Symptoms". Mayo Clinic.
- ↑ "ISDA MRSA guidelines" (PDF).
- ↑ "MRSA Toxin Acquitted: Study Clears Suspected Key to Severe Bacterial Illness". NIH news release. National Institute of Health. 2006-11-06.
- 1 2 Raygada JL, Levine DP (March 30, 2009). "Managing CA-MRSA Infections: Current and Emerging Options". Infections in Medicine. 26 (2).
- 1 2 3 "General Information About MRSA in the Community". Centers for Disease Control and Prevention. 10 September 2013. Retrieved 9 October 2014.
- ↑ Lipsky BA, Tabak YP, Johannes RS, Vo L, Hyde L, Weigelt JA (May 2010). "Skin and soft tissue infections in hospitalised patients with diabetes: culture isolates and risk factors associated with mortality, length of stay and cost". Diabetologia. 53 (5): 914–23. doi:10.1007/s00125-010-1672-5. PMID 20146051.
- ↑ Otter, J.A.; French, G.L. "Community-associated meticillin-resistant Staphylococcus aureus strains as a cause of healthcare-associated infection". Journal of Hospital Infection. 79 (3): 189–193. doi:10.1016/j.jhin.2011.04.028.
- ↑ Golding, George R.; Quinn, Brian; Bergstrom, Kirsten; Stockdale, Donna; Woods, Shirley; Nsungu, Mandiangu; Brooke, Barb; Levett, Paul N.; Horsman, Greg; McDonald, Ryan; Szklarczuk, Brian; Silcox, Steve; Paton, Shirley; Carson, Mary; Mulvey, Michael R.; Irvine, James. "Community-based educational intervention to limit the dissemination of community-associated methicillin-resistant Staphylococcus aureus in Northern Saskatchewan, Canada". BMC Public Health. 12 (1): 15. doi:10.1186/1471-2458-12-15.
- 1 2 3 Tacconelli E, De Angelis G, Cataldo MA, Pozzi E, Cauda R (Jan 2008). "Does antibiotic exposure increase the risk of methicillin-resistant Staphylococcus aureus (MRSA) isolation? A systematic review and meta-analysis". J Antimicrob Chemother. 61 (1): 26–38. doi:10.1093/jac/dkm416. PMID 17986491.
- ↑ Elias, Johannes; Heuschmann, Peter U.; Schmitt, Corinna; Eckhardt, Frithjof; Boehm, Hartmut; Maier, Sebastian; Kolb-Mäurer, Annette; Riedmiller, Hubertus; Müllges, Wolfgang; Weisser, Christoph; Wunder, Christian; Frosch, Matthias; Vogel, Ulrich (February 2013). "Prevalence dependent calibration of a predictive model for nasal carriage of methicillin-resistant Staphylococcus aureus". BMC Infectious Diseases. 13 (111): 1–12. doi:10.1186/1471-2334-13-111. Retrieved 2014-10-07.
- ↑ Reuters (2009-02-16). "Study: Beachgoers More Likely to Catch MRSA". FoxNews.com.
- ↑ Marilynn Marchione (2009-09-12). "Dangerous staph germs found at West Coast beaches". Associated Press.
- ↑ Zinderman CE, Conner B, Malakooti MA, LaMar JE, Armstrong A, Bohnker BK (May 2004). "Community-Acquired Methicillin-Resistant Staphylococcus aureus Among Military Recruits". Emerging Infectious Diseases. 10 (5): 941–4. doi:10.3201/eid1005.030604. PMC 3323224
 . PMID 15200838.
. PMID 15200838. - 1 2 David MZ, Daum RS (2010). "Community-Associated Methicillin-Resistant Staphylococcus aureus: Epidemiology and Clinical Consequences of an Emerging Epidemic" (PDF). Clinical Microbiology Reviews. American Society for Microbiology. 23 (6): 616–687. doi:10.1128/CMR.00081-09. PMC 2901661
 . PMID 20610826.
. PMID 20610826. - 1 2 Muto CA, Jernigan JA, Ostrowsky BE, Richet HM, Jarvis WR, Boyce JM, Farr BM (May 2003). "SHEA guideline for preventing nosocomial transmission of multidrug-resistant strains of Staphylococcus aureus and enterococcus". Infect Control Hosp Epidemiol. 24 (5): 362–86. doi:10.1086/502213. PMID 12785411.
- ↑ Johannes Elias (September 2014). "Predict probability of MRSA carriage in hospital admissions". Retrieved 2014-10-07.
- ↑ "PURE Bioscience". purebio.com.
- ↑ "Joint scientific report of ECDC, EFSA and EMEA on meticillin resistant Staphylococcus aureus (MRSA) in livestock, companion animals and food" (PDF). 2009-06-16. Retrieved 2009-09-19.
- ↑ Harrison, Ewan M.; Paterson, Gavin K.; Holden, Matthew T.G.; Larsen, Jesper; Stegger, Marc; Larsen, Anders Rhod; Petersen, Andreas; Skov, Robert L.; et al. (2013). "Whole genome sequencing identifies zoonotic transmission of MRSA isolates with the novel mecA homologue mecC". EMBO Molecular Medicine. 5 (4): 509–15. doi:10.1002/emmm.201202413. PMC 3628104
 . PMID 23526809.
. PMID 23526809. - ↑ Tomasz, Alexander (April 2013). "The use of whole genome sequencing to solve an epidemiological puzzle". EMBO Molecular Medicine. 5 (4): 486–487. doi:10.1002/emmm.201302622.
- ↑ "US meat and poultry is widely contaminated with drug-resistant Staph bacteria, study finds". ScienceDaily.
- ↑ Ogata K, Narimatsu H, Suzuki M, Higuchi W, Yamamoto T, Taniguchi H (2012-02-03). "Commercially distributed meat as a potential vehicle for community-acquired methicillin-resistant Staphylococcus aureus". Applied and Environmental Microbiology. 78 (8): 2797–802. doi:10.1128/AEM.07470-11. PMC 3318828
 . PMID 22307310.
. PMID 22307310. - ↑ Harvey, Fiona; Carson, Mary; O'Kane, Maggie; Wasley, Andrew (18 June 2015). "MRSA superbug found in supermarket pork raises alarm over farming risks". The Guardian.
- ↑ Salgado, Cassandra D.; Farr, Barry M.; Calfee, David P. (15 January 2003). "Community‐Acquired Methicillin‐Resistant Staphylococcus aureus: A Meta‐Analysis of Prevalence and Risk Factors". Clinical Infectious Diseases. 36 (2): 131–139. doi:10.1086/345436.
- ↑ Kazakova SV, Hageman JC, Matava M, Srinivasan A, Phelan L, Garfinkel B, Boo T, McAllister S, Anderson J, Jensen B, Dodson D, Lonsway D, McDougal LK, Arduino M, Fraser VJ, Killgore G, Tenover FC, Cody S, Jernigan DB (2005-02-03). "A clone of methicillin-resistant Staphylococcus aureus among professional football players". The New England Journal of Medicine. 352 (5): 468–75. doi:10.1056/NEJMoa042859. PMID 15689585.
- ↑ Epstein, Victor (21 December 2007). "Texas Football Succumbs to Virulent Staph Infection From Turf". Bloomberg. Retrieved 10 June 2010.
- ↑ Yasinskas, Pat (11 October 2013). "Third Tampa Bay Buccaneers player tests positive for MRSA staph infection". ESPN. ESPN Internet Ventures. Retrieved 11 October 2013.
- ↑ Hernandez, Dylan (August 12, 2015). "Dodgers' Justin Turner nears return from MRSA infection". Los Angeles Times. Retrieved August 13, 2015.
- ↑ Rappoport, Ian (October 11, 2015). "MRSA infection leaves Giants' Daniel Fells in dire situation". NFL.com. Retrieved October 12, 2015.
- ↑ Gray JW (April 2004). "MRSA: the problem reaches paediatrics". Arch. Dis. Child. 89 (4): 297–8. doi:10.1136/adc.2003.045534. PMC 1719885
 . PMID 15033832.
. PMID 15033832. - ↑ Bratu S, Eramo A, Kopec R, Coughlin E, Ghitan M, Yost R, Chapnick EK, Landman D, Quale J (June 2005). "Community-associated methicillin-resistant Staphylococcus aureus in hospital nursery and maternity units". Emerging Infect. Dis. 11 (6): 808–13. doi:10.3201/eid1106.040885. PMC 3367583
 . PMID 15963273.
. PMID 15963273. - ↑ Association for Professionals in Infection Control & Epidemiology (June 25, 2007). "National Prevalence Study of Methicillin-Resistant Staphylococcus aureus (MRSA) in U.S. Healthcare Facilities". Archived from the original on September 7, 2007. Retrieved 2007-07-14.
- ↑ "Staph Infections and MRSA in Children: Prevention, Symptoms, and Treatment". webmd.com.
- ↑ Ceylan Koydemir H, Külah H, Özgen C, Alp A, Hasçelik G (2011). "MEMS biosensors for detection of methicillin resistant Staphylococcus aureus". Biosensors and Bioelectronics. 29 (1): 1–12. doi:10.1016/j.bios.2011.07.071. PMID 21856144.
- ↑ Francois P, Schrenzel J (2008). "Rapid Diagnosis and Typing of Staphylococcus aureus". Staphylococcus: Molecular Genetics. Caister Academic Press. ISBN 978-1-904455-29-5.
- ↑ Mackay IM, ed. (2007). Real-Time PCR in Microbiology: From Diagnosis to Characterization. Caister Academic Press. ISBN 978-1-904455-18-9.
- ↑ Seiken, Denka. "MRSA latex test for PBP2".
- 1 2 3 4 5 Jensen SO, Lyon BR (June 2009). "Genetics of antimicrobial resistance in Staphylococcus aureus". Future Microbiol. 4 (5): 565–82. doi:10.2217/fmb.09.30. PMID 19492967.
- 1 2 3 4 5 6 7 8 9 Lowy FD (May 2003). "Antimicrobial resistance: the example of Staphylococcus aureus". J. Clin. Invest. 111 (9): 1265–73. doi:10.1172/JCI18535. PMC 154455
 . PMID 12727914.
. PMID 12727914. - 1 2 3 4 5 6 Pantosti A, Sanchini A, Monaco M (June 2007). "Mechanisms of antibiotic resistance in Staphylococcus aureus". Future Microbiol. 2 (3): 323–34. doi:10.2217/17460913.2.3.323. PMID 17661706.
- ↑ Kaito C, Saito Y, Nagano G, Ikuo M, Omae Y, Hanada Y, Han X, Kuwahara-Arai K, Hishinuma T, Baba T, Ito T, Hiramatsu K, Sekimizu K (2011). Cheung A, ed. "Transcription and translation products of the cytolysin gene psm-mec on the mobile genetic element SCCmec regulate Staphylococcus aureus virulence". PLoS Pathog. 7 (2): e1001267. doi:10.1371/journal.ppat.1001267. PMC 3033363
 . PMID 21304931.
. PMID 21304931. - ↑ Enright, M.C.; Robinson, D.A. (2002). "The evolutionary history of methicillin-resistant Staphylococcus aureus (MRSA).". PNAS. 99.
- ↑ Wu, S.W.; de Lencastre, H. (2001). "Recruitment of the mecA gene homolog of Staphyoloccus sciuri into a resistance determinant and expression of the resistance phenotype in Staphylococcus aureus". Journal of Bacteriology. 183.
- 1 2 3 Kuo SC, Chiang MC, Lee WS, Chen LY, Wu HS, Yu KW, Fung CP, Wang FD (January 2012). "Comparison of microbiological and clinical characteristics based on SCCmec typing in patients with community-onset meticillin-resistant Staphylococcus aureus (MRSA) bacteraemia". Int. J. Antimicrob. Agents. 39 (1): 22–6. doi:10.1016/j.ijantimicag.2011.08.014. PMID 21982834.
- 1 2 3 Collins, J.; Rudkin, J. (2010). "Offsetting virulence and antibiotic resistance costs by MRSA". International Society for Microbial Ecology. 4.
- ↑ Sahebnasagh R, Saderi H, Owlia P. Detection of methicillin-resistant Staphylococcus aureus strains from clinical samples in Tehran by detection of the mecA and nuc genes. The First Iranian International Congress of Medical Bacteriology; 4–7 September; Tabriz, Iran. 2011. 195 pp.
- 1 2 Berger-Bächi B (November 1999). "Genetic basis of methicillin resistance in Staphylococcus aureus". Cell. Mol. Life Sci. 56 (9–10): 764–70. doi:10.1007/s000180050023. PMID 11212336.
- ↑ Goering RV, McDougal LK, Fosheim GE, Bonnstetter KK, Wolter DJ, Tenover FC (2007). "Epidemiologic distribution of the arginine catabolic mobile element among selected methicillin-resistant and methicillin-susceptible Staphylococcus aureus isolates". J. Clin. Microbiol. 45 (6): 1981–4. doi:10.1128/JCM.00273-07. PMC 1933090
 . PMID 17409207.
. PMID 17409207. - 1 2 3 4 5 6 7 Gordon RJ, Lowy FD (June 2008). "Pathogenesis of methicillin-resistant Staphylococcus aureus infection". Clin. Infect. Dis. 46 (Suppl 5): S350–9. doi:10.1086/533591. PMC 2474459
 . PMID 18462090.
. PMID 18462090. - ↑ Johnson AP, Aucken HM, Cavendish S, Ganner M, Wale MC, Warner M, Livermore DM, Cookson BD (2001). "Dominance of EMRSA-15 and -16 among MRSA causing nosocomial bacteraemia in the UK: analysis of isolates from the European Antimicrobial Resistance Surveillance System (EARSS)". J Antimicrob Chemother. 48 (1): 143–4. doi:10.1093/jac/48.1.143. PMID 11418528.
- ↑ Holden MT, Feil EJ, Lindsay JA, Peacock SJ, Day NP, Enright MC, Foster TJ, Moore CE, Hurst L, Atkin R, Barron A, Bason N, Bentley SD, Chillingworth C, Chillingworth T, Churcher C, Clark L, Corton C, Cronin A, Doggett J, Dowd L, Feltwell T, Hance Z, Harris B, Hauser H, Holroyd S, Jagels K, James KD, Lennard N, Line A, Mayes R, Moule S, Mungall K, Ormond D, Quail MA, Rabbinowitsch E, Rutherford K, Sanders M, Sharp S, Simmonds M, Stevens K, Whitehead S, Barrell BG, Spratt BG, Parkhill J (2004). "Complete genomes of two clinical Staphylococcus aureus strains: Evidence for the rapid evolution of virulence and drug resistance". Proc Natl Acad Sci USA. 101 (26): 9786–91. doi:10.1073/pnas.0402521101. PMC 470752
 . PMID 15213324.
. PMID 15213324. - 1 2 Diep BA, Carleton HA, Chang RF, Sensabaugh GF, Perdreau-Remington F (2006). "Roles of 34 virulence genes in the evolution of hospital- and community-associated strains of methicillin-resistant Staphylococcus aureus". J Infect Dis. 193 (11): 1495–503. doi:10.1086/503777. PMID 16652276.
- 1 2 Stefani S, Chung DR, Lindsay JA, Friedrich AW, Kearns AM, Westh H, Mackenzie FM (2012). "Meticillin-resistant Staphylococcus aureus (MRSA): global epidemiology and harmonisation of typing methods". International Journal of Antimicrobial Agents. 39 (4): 273–82. doi:10.1016/j.ijantimicag.2011.09.030. ISSN 0924-8579. PMID 22230333.
- 1 2 3 4 5 6 Calfee DP (2011). "The epidemiology, treatment, and prevention of transmission of methicillin-resistant Staphylococcus aureus". J Infus Nurs. 34 (6): 359–64. doi:10.1097/NAN.0b013e31823061d6. PMID 22101629.
- ↑ von Eiff C, Becker K, Metze D, Lubritz G, Hockmann J, Schwarz T, Peters G (2001). "Intracellular persistence of Staphylococcus aureus small-colony variants within keratinocytes: a cause for antibiotic treatment failure in a patient with Darier's disease". Clin Infect Dis. 32 (11): 1643–7. doi:10.1086/320519. PMID 11340539.
- ↑ Clement S, Vaudaux P, Francois P, Schrenzel J, Huggler E, Kampf S, Chaponnier C, Lew D, Lacroix JS (2005). "Evidence of an intracellular reservoir in the nasal mucosa of patients with recurrent Staphylococcus aureus rhinosinusitis". J Infect Dis. 192 (6): 1023–8. doi:10.1086/432735. PMID 16107955.
- ↑ Zautner AE, Krause M, Stropahl G, Holtfreter S, Frickmann H, Maletzki C, Kreikemeyer B, Pau HW, Podbielski A (2010). Bereswill S, ed. "Intracellular persisting Staphylococcus aureus is the major pathogen in recurrent tonsillitis". PLOS ONE. 5 (3): e9452. doi:10.1371/journal.pone.0009452. PMC 2830486
 . PMID 20209109.
. PMID 20209109. - ↑ "New Study finds MRSA on the rise in hospital outpatients". 2009.
- ↑ Daum RS (2007). "Skin and Soft-Tissue Infections Caused by Methicillin-Resistant Staphylococcus aureus". New England Journal of Medicine. 357 (4): 380–390. doi:10.1056/NEJMcp070747. PMID 17652653.
- ↑ Wang R, Braughton KR, Kretschmer D, Bach TH, Queck SY, Li M, Kennedy AD, Dorward DW, Klebanoff SJ, Peschel A, DeLeo FR, Otto M (December 2007). "Identification of novel cytolytic peptides as key virulence determinants for community-associated MRSA". Nat. Med. 13 (12): 1510–4. doi:10.1038/nm1656. PMID 17994102.
- ↑ Tristan A, Bes M, Meugnier H, Lina G, Bozdogan B, Courvalin P, Reverdy ME, Enright MC, Vandenesch F, Etienne J (2007). "Global distribution of Panton–Valentine leukocidin--positive methicillin-resistant Staphylococcus aureus, 2006". Emerging Infect. Dis. 13 (4): 594–600. doi:10.3201/eid1304.061316. PMC 2725977
 . PMID 17553275.
. PMID 17553275. - ↑ Gould IM, David MZ, Esposito S, Garau J, Lina G, Mazzei T, Peters G (February 2012). "New insights into meticillin-resistant Staphylococcus aureus (MRSA) pathogenesis, treatment and resistance". Int. J. Antimicrob. Agents. 39 (2): 96–104. doi:10.1016/j.ijantimicag.2011.09.028. PMID 22196394.
- ↑ David MZ, Rudolph KM, Hennessy TW, Boyle-Vavra S, Daum RS (2008). "Molecular epidemiology of methicillin-resistant Staphylococcus aureus, rural southwestern Alaska". Emerging Infect. Dis. 14 (11): 1693–9. doi:10.3201/eid1411.080381. PMC 2630737
 . PMID 18976551.
. PMID 18976551. - ↑ Ahlstrom, Dick (2011-06-03). "New strain of MRSA superbug discovered in Dublin hospitals". The Irish Times.
- ↑ Graveland H, Duim B, van Duijkeren E, Heederik D, Wagenaar JA (December 2011). "Livestock-associated methicillin-resistant Staphylococcus aureus in animals and humans". Int. J. Med. Microbiol. 301 (8): 630–4. doi:10.1016/j.ijmm.2011.09.004. PMID 21983338.
- ↑ Tacconelli E, De Angelis G, de Waure C, Cataldo MA, La Torre G, Cauda R (September 2009). "Rapid screening tests for meticillin-resistant Staphylococcus aureus at hospital admission: systematic review and meta-analysis". Lancet Infect Dis. 9 (9): 546–54. doi:10.1016/S1473-3099(09)70150-1. PMID 19695491.
- ↑ "To Catch a Deadly Germ," New York Times opinion
- ↑ "Healthcare-associated infections - HAI - CDC" (PDF). cdc.gov.
- ↑ Archived April 2, 2009, at the Wayback Machine.
- ↑ "MRSA test for surgical patients". BBC News. 2009-03-31. Retrieved 2010-04-05.
- ↑ Home Mrsa Test - Home
- ↑ Fritz SA, Garbutt J, Elward A, Shannon W, Storch GA (2008). "Prevalence of and risk factors for community-acquired methicillin-resistant and methicillin-sensitive Staphylococcus aureus colonization in children seen in a practice-based research network". Pediatrics. 121 (6): 1090–8. doi:10.1542/peds.2007-2104. PMID 18519477.
- ↑ Otter JA, Puchowicz M, Ryan D, Salkeld JA, Cooper TA, Havill NL, Tuozzo K, Boyce JM (June 2009). "Feasibility of routinely using hydrogen peroxide vapor to decontaminate rooms in a busy United States hospital". Infect Control Hosp Epidemiol. 30 (6): 574–7. doi:10.1086/597544. PMID 19415969.
- ↑ Bartels MD, Kristoffersen K, Slotsbjerg T, Rohde SM, Lundgren B, Westh H (September 2008). "Environmental meticillin-resistant Staphylococcus aureus (MRSA) disinfection using dry-mist-generated hydrogen peroxide". J. Hosp. Infect. 70 (1): 35–41. doi:10.1016/j.jhin.2008.05.018. PMID 18621434.
- ↑ French GL, Otter JA, Shannon KP, Adams NM, Watling D, Parks MJ (May 2004). "Tackling contamination of the hospital environment by methicillin-resistant Staphylococcus aureus (MRSA): a comparison between conventional terminal cleaning and hydrogen peroxide vapour decontamination". J. Hosp. Infect. 57 (1): 31–7. doi:10.1016/j.jhin.2004.03.006. PMID 15142713.
- ↑ Otter JA, Cummins M, Ahmad F, van Tonder C, Drabu YJ (October 2007). "Assessing the biological efficacy and rate of recontamination following hydrogen peroxide vapour decontamination". J. Hosp. Infect. 67 (2): 182–8. doi:10.1016/j.jhin.2007.07.019. PMID 17884250.
- ↑ Hardy KJ, Gossain S, Henderson N, Drugan C, Oppenheim BA, Gao F, Hawkey PM (August 2007). "Rapid recontamination with MRSA of the environment of an intensive care unit after decontamination with hydrogen peroxide vapour". J. Hosp. Infect. 66 (4): 360–8. doi:10.1016/j.jhin.2007.05.009. PMID 17655975.
- ↑ Omidbakhsh N, Sattar SA (June 2006). "Broad-spectrum microbicidal activity, toxicologic assessment, and materials compatibility of a new generation of accelerated hydrogen peroxide-based environmental surface disinfectant". Am J Infect Control. 34 (5): 251–7. doi:10.1016/j.ajic.2005.06.002. PMID 16765201.
- ↑ Michels HT, Noyce JO, Keevil CW (2009). "Effects of temperature and humidity on the efficacy of methicillin-resistant Staphylococcus aureus challenged antimicrobial materials containing silver and copper" (PDF). Letters in Applied Microbiology. 49 (2): 191–5. doi:10.1111/j.1472-765X.2009.02637.x. PMC 2779462
 . PMID 19413757.
. PMID 19413757. - ↑ Keevil, C.W., Noyce, J.O. (2007), Antimicrobial Efficacies of Copper, Stainless Steel, Microban, BioCote and AgIon with MRSA at 20 °C, unpublished data
- ↑ Noyce, J.O. and Keevil, C.W. (2004), The Antimicrobial Effects of Copper and Copper-Based Alloys on Methicillin-resistant Staphylococcus aureus, Copper Development Association Poster Q-193 from Proceedings of the Annual General Meeting of the American Society for Microbiology, 24–27 May 2004, New Orleans; presented at the American Society for Microbiology General Meeting, New Orleans, LA May 24th.
- ↑ "NPSA - About us".
- ↑ DeMarco CE, Cushing LA, Frempong-Manso E, Seo SM, Jaravaza TA, Kaatz GW (Sep 2007). "Efflux-Related Resistance to Norfloxacin, Dyes, and Biocides in Bloodstream Isolates of Staphylococcus aureus" (Free full text). Antimicrobial Agents and Chemotherapy. 51 (9): 3235–3239. doi:10.1128/AAC.00430-07. ISSN 0066-4804. PMC 2043220
 . PMID 17576828.
. PMID 17576828. - ↑ Haley CE, Marling-Cason M, Smith JW, Luby JP, Mackowiak PA (June 1985). "Bactericidal activity of antiseptics against methicillin-resistant Staphylococcus aureus". J. Clin. Microbiol. 21 (6): 991–2. PMC 271835
 . PMID 4008627.
. PMID 4008627. - ↑ "Simple techniques slash hospital infections: meeting". Reuters. 2009-03-21.
- 1 2 3 "NIOSH MRSA and the Workplace". United States National Institute for Occupational Safety and Health. Retrieved 2007-10-29.
- ↑ CDC (1998). "Guidelines for Infection Control in Health Care Personnel, 1998". Centers for Disease Control and Prevention. Retrieved December 18, 2007.
- ↑ Eili Y. Klein; Lova Sun; David L. Smith; Ramanan Laxminarayan (2013). "The Changing Epidemiology of Methicillin-Resistant Staphylococcus aureus in the United States: A National Observational Study". American Journal of Epidemiology. 177 (7): 666–674. doi:10.1093/aje/kws273.
- ↑ http://www.cdc.gov/drugresistance/threat-report-2013/
- ↑ Cooper BS, Medley GF, Stone SP, Kibbler CC, Cookson BD, Roberts JA, Duckworth G, Lai R, Ebrahim S (2004). "Methicillin-resistant Staphylococcus aureus in hospitals and the community: stealth dynamics and control catastrophes". Proc Natl Acad Sci USA. 101 (27): 10223–8. doi:10.1073/pnas.0401324101. PMC 454191
 . PMID 15220470.
. PMID 15220470. - ↑ Bootsma MC, Diekmann O, Bonten MJ (2006). "Controlling methicillin-resistant Staphylococcus aureus: quantifying the effects of interventions and rapid diagnostic testing". Proc Natl Acad Sci USA. 103 (14): 5620–5. doi:10.1073/pnas.0510077103. PMC 1459403
 . PMID 16565219.
. PMID 16565219. - ↑ Klevens RM, Edwards JR, Richards CL, Horan TC, Gaynes RP, Pollock DA, Cardo DM (2007). "Estimating health care-associated infections and deaths in U.S. hospitals, 2002". Public Health Rep. 122 (2): 160–6. PMC 1820440
 . PMID 17357358.
. PMID 17357358. - ↑ Hidron AI, Edwards JR, Patel J, Horan TC, Sievert DM, Pollock DA, Fridkin SK (November 2008). "NHSN annual update: antimicrobial-resistant pathogens associated with healthcare-associated infections: annual summary of data reported to the National Healthcare Safety Network at the Centers for Disease Control and Prevention, 2006-2007". Infect Control Hosp Epidemiol. 29 (11): 996–1011. doi:10.1086/591861. PMID 18947320.
- ↑ Johnson AP, Pearson A, Duckworth G (2005). "Surveillance and epidemiology of MRSA bacteraemia in the UK". J Antimicrob Chemother. 56 (3): 455–62. doi:10.1093/jac/dki266. PMID 16046464.
- ↑ Inquirer.net, Cases of RP maids with 'superbug' infection growing in HK
- ↑ "MRSA Infections". Keep Kids Healthy.
- ↑ Graham PL, Lin SX, Larson EL (2006). "A U.S. population-based survey of Staphylococcus aureus colonization". Annals of Internal Medicine. 144 (5): 318–25. doi:10.7326/0003-4819-144-5-200603070-00006. PMID 16520472.
- ↑ Jernigan JA, Arnold K, Heilpern K, Kainer M, Woods C, Hughes JM (2006-05-12). "Methicillin-resistant Staphylococcus aureus as community pathogen". Symposium on Community-Associated Methicillin-resistant Staphylococcus aureus (Atlanta, Georgia, U.S.). Cited in Emerg Infect Dis. Centers for Disease Control and Prevention. Retrieved 2007-01-27.
- ↑ First study finds MRSA in U.S. pigs and farmers, seattlepi.com, 4 June 2008
- ↑ Our Pigs, Our Food, Our Health, The New York Times, 12 March 2009
- 1 2 "PubMed Health". US National Institutes of Health. Retrieved 20 November 2011.
- ↑ "Optimal Bleach Concentration Required to Kill MRSA in Bath Water". American Academy of Pediatrics. Retrieved 23 August 2013.
- 1 2 "Living With MRSA" (PDF). Group Health Cooperative/Tacoma-Pierce County Health Dept./Washington State Dept. of Health. Retrieved 20 November 2011.
- ↑ Shi CM, Nakao H, Yamazaki M, Tsuboi R, Ogawa H (November 2007). "Mixture of sugar and povidone-iodine stimulates healing of MRSA-infected skin ulcers on db/db mice". Arch. Dermatol. Res. 299 (9): 449–56. doi:10.1007/s00403-007-0776-3. PMID 17680256.
- ↑ "THE NOSE – "GROUND ZERO" FOR MRSA COLONIZATION". Ondine Biomedical Inc. Retrieved 20 November 2011.
- ↑ "Personal Prevention of MRSA Skin Infections". CDC. 9 August 2010.
- ↑ The Provision of Public Toilets
- ↑ Government Response to the Communities and Local Government Committee Report on the Provision of Public Toilets
- ↑ "Clinical Practice Guidelines by the Infectious Diseases Society of America for the Treatment of Methicillin-Resistant Staphylococcus Aureus Infections in Adults and Children" (PDF).
- ↑ "FDA Approves Teflaro for Bacterial Infections".
- ↑ Schentag JJ, Hyatt JM, Carr JR, Paladino JA, Birmingham MC, Zimmer GS, Cumbo TJ (1998). "Genesis of methicillin-resistant Staphylococcus aureus (MRSA), how treatment of MRSA infections has selected for vancomycin-resistant Enterococcus faecium, and the importance of antibiotic management and infection control". Clin. Infect. Dis. 26 (5): 1204–14. doi:10.1086/520287. PMID 9597254.
- ↑ Rybak MJ, Lerner SA, Levine DP, Albrecht LM, McNeil PL, Thompson GA, Kenny MT, Yuh L (1991). "Teicoplanin pharmacokinetics in intravenous drug abusers being treated for bacterial endocarditis". Antimicrob. Agents Chemother. 35 (4): 696–700. doi:10.1128/AAC.35.4.696. PMC 245081
 . PMID 1829880.
. PMID 1829880. - ↑ Janknegt R (1997). "The treatment of staphylococcal infections with special reference to pharmacokinetic, pharmacodynamic, and pharmacoeconomic considerations". Pharmacy world & science: PWS. 19 (3): 133–41. doi:10.1023/A:1008609718457. PMID 9259029.
- ↑ Chang FY, Peacock JE, Musher DM, Triplett P, MacDonald BB, Mylotte JM, O'Donnell A, Wagener MM, Yu VL (2003). "Staphylococcus aureus bacteremia: recurrence and the impact of antibiotic treatment in a prospective multicenter study". Medicine (Baltimore). 82 (5): 333–9. doi:10.1097/01.md.0000091184.93122.09. PMID 14530782.
- ↑ Siegman-Igra Y, Reich P, Orni-Wasserlauf R, Schwartz D, Giladi M (2005). "The role of vancomycin in the persistence or recurrence of Staphylococcus aureus bacteraemia". Scand J Infect Dis. 37 (8): 572–8. doi:10.1080/00365540510038488. PMID 16138425.
- ↑ Sieradzki K, Tomasz A (1997). "Inhibition of cell wall turnover and autolysis by vancomycin in a highly vancomycin-resistant mutant of Staphylococcus aureus". J. Bacteriol. 179 (8): 2557–66. PMC 179004
 . PMID 9098053.
. PMID 9098053. - ↑ Schito GC (2006). "The importance of the development of antibiotic resistance in Staphylococcus aureus". Clin Microbiol Infect. 12 (Suppl 1): 3–8. doi:10.1111/j.1469-0691.2006.01343.x. PMID 16445718.
- ↑ Mongkolrattanothai K, Boyle S, Kahana MD, Daum RS (2003). "Severe Staphylococcus aureus infections caused by clonally related community-associated methicillin-susceptible and methicillin-resistant isolates". Clin. Infect. Dis. 37 (8): 1050–8. doi:10.1086/378277. PMID 14523769.
- ↑ Liu C, Bayer A, Cosgrove SE, Daum RS, Fridkin SK, Gorwitz RJ, Kaplan SL, Karchmer AW, Levine DP, Murray BE, J Rybak M, Talan DA, Chambers HF (Feb 1, 2011). "Clinical practice guidelines by the Infectious Diseases Society of America for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children: executive summary". Clin Infect Dis. 61 (2): 285–92. doi:10.1093/cid/cir034. PMID 21217178.
- 1 2 3 4 "MRSA History Timeline: The First Half-Century, 1959-2009". The University of Chicago Medical Center. 2010.
- 1 2 3 "MRSA Surveillance". Centers for Disease Control and Prevention. April 8, 2011.
- ↑ Community-acquired MRSA in Children with no predisposing risk
- ↑ UK Office for National Statistics Online (February 22, 2007), "MRSA Deaths continue to rise in 2005"
- ↑ Hospitals struck by new killer bug An article by Manchester free newspaper 'Metro', May 7, 2008
- ↑ Blot SI, Vandewoude KH, Hoste EA, Colardyn FA (2002). "Outcome and attributable mortality in critically Ill patients with bacteremia involving methicillin-susceptible and methicillin-resistant Staphylococcus aureus". Arch Intern Med. 162 (19): 2229–35. doi:10.1001/archinte.162.19.2229. PMID 12390067.
- ↑ Liu C, Graber CJ, Karr M, Diep BA, Basuino L, Schwartz BS, Enright MC, O'Hanlon SJ, Thomas JC, Perdreau-Remington F, Gordon S, Gunthorpe H, Jacobs R, Jensen P, Leoung G, Rumack JS, Chambers HF (June 2008). "A population-based study of the incidence and molecular epidemiology of methicillin-resistant Staphylococcus aureus disease in San Francisco, 2004–2005". Clin. Infect. Dis. 46 (11): 1637–46. doi:10.1086/587893. PMID 18433335.
- ↑ Noskin GA, Rubin RJ, Schentag JJ, Kluytmans J, Hedblom EC, Smulders M, Lapetina E, Gemmen E (2005). "The Burden of Staphylococcus aureus Infections on Hospitals in the United States: An Analysis of the 2000 and 2001 Nationwide Inpatient Sample Database". Arch Intern Med. 165 (15): 1756–1761. doi:10.1001/archinte.165.15.1756. PMID 16087824.
- ↑ Cosgrove SE, Qi Y, Kaye KS, Harbarth S, Karchmer AW, Carmeli Y (2005). "The impact of Methicillin Resistance in Staphylococcus aureus Bacteremia on Patient Outcomes: Mortality, Length of Stay, and Hospital Charges". Infection Control and Hospital Epidemiology. 26 (2): 166–174. doi:10.1086/502522. PMID 15756888.
- ↑ Hardy KJ, Hawkey PM, Gao F, Oppenheim BA (2004). "Methicillin resistant Staphylococcus aureus in the critically ill". British Journal of Anaesthesia. 92 (1): 121–30. doi:10.1093/bja/aeh008. PMID 14665563.
- ↑ Wyllie DH, Crook DW, Peto TE (2006). "Mortality after Staphylococcus aureus bacteraemia in two hospitals in Oxfordshire, 1997–2003: cohort study". BMJ. 333 (7562): 281. doi:10.1136/bmj.38834.421713.2F. PMC 1526943
 . PMID 16798756.
. PMID 16798756. - ↑ "Outcomes in EHCI 2015" (PDF). Health Consumer Powerhouse. 26 January 2016. Retrieved 27 January 2016.
- ↑ "Tools". cddep.org.
- 1 2 "Outcomes in EHCI 2015" (PDF). Health Consumer Powerhouse. 26 January 2016. Retrieved 27 January 2016.
- ↑ Clinical trial number NCT00685698 for "Safety and Efficacy Study of TG-873870 (Nemonoxacin) in Diabetic Foot Infections" at ClinicalTrials.gov
- ↑ "Novartis Stops Development of Aurograb". Drug Discovery and Development. August 29, 2008.
- ↑ Bowling FL, Salgami EV, Boulton AJ (2007). "Larval therapy: a novel treatment in eliminating methicillin-resistant Staphylococcus aureus from diabetic foot ulcers". Diabetes Care. 30 (2): 370–1. doi:10.2337/dc06-2348. PMID 17259512.
- ↑ "Maggots help cure MRSA patients". BBC News. 2007-05-02.
- ↑ "Maggots rid patients of MRSA". EurekAlert!/AAAS. 2007-05-03.
- ↑ Murphy, Clare (2007-08-13). "'Red Army' virus to combat MRSA". BBC News.
- ↑ Matsuzaki S, Yasuda M, Nishikawa H, Kuroda M, Ujihara T, Shuin T, Shen Y, Jin Z, Fujimoto S, Nasimuzzaman MD, Wakiguchi H, Sugihara S, Sugiura T, Koda S, Muraoka A, Imai S (2003). "Experimental protection of mice against lethal Staphylococcus aureus infection by novel bacteriophage phi MR11". J. Infect. Dis. 187 (4): 613–24. doi:10.1086/374001. PMID 12599078.
- ↑ Bayston R, Ashraf W, Smith T (2007). "Triclosan resistance in methicillin-resistant Staphylococcus aureus expressed as small colony variants: a novel mode of evasion of susceptibility to antiseptics". J. Antimicrob. Chemother. 59 (5): 848–53. doi:10.1093/jac/dkm031. PMID 17337510.
- ↑ Wang J, Soisson SM, Young K, Shoop W, Kodali S, Galgoci A, Painter R, Parthasarathy G, Tang YS, Cummings R, Ha S, Dorso K, Motyl M, Jayasuriya H, Ondeyka J, Herath K, Zhang C, Hernandez L, Allocco J, Basilio A, Tormo JR, Genilloud O, Vicente F, Pelaez F, Colwell L, Lee SH, Michael B, Felcetto T, Gill C, Silver LL, Hermes JD, Bartizal K, Barrett J, Schmatz D, Becker JW, Cully D, Singh SB (May 2006). "Platensimycin is a selective FabF inhibitor with potent antibiotic properties". Nature. 441 (7091): 358–361. doi:10.1038/nature04784. PMID 16710421.
- ↑ Mullin, Emily (11 March 2014). "University of Notre Dame team IDs new class of antibiotics". fiercebiotechresearch.com. Retrieved 19 March 2014.
- ↑ O'Daniel PI, Peng Z, Pi H, Testero SA, Ding D, Spink E, Leemans E, Boudreau MA, Yamaguchi T, Schroeder VA, Wolter WR, Llarrull LI, Song W, Lastochkin E, Kumarasiri M, Antunes NT, Espahbodi M, Lichtenwalter K, Suckow MA, Vakulenko S, Mobashery S, Chang M (2014). "Discovery of a New Class of Non-β-lactam Inhibitors of Penicillin-Binding Proteins with Gram-Positive Antibacterial Activity". J. Am. Chem. Soc. ACS. 136 (9): 3664–3672. doi:10.1021/ja500053x. PMID 24517363.
- ↑ Sherlock O, Dolan A, Athman R, Power A, Gethin G, Cowman S, Humphreys H (2010). "Comparison of the antimicrobial activity of Ulmo honey from Chile and Manuka honey against methicillin-resistant Staphylococcus aureus, Escherichia coli and Pseudomonas aeruginosa". BMC Complement Altern Med. 10: 47. doi:10.1186/1472-6882-10-47. PMC 2942791
 . PMID 20813024.
. PMID 20813024. - ↑ Kwakman PH, te Velde AA, de Boer L, Speijer D, Vandenbroucke-Grauls CM, Zaat SA (July 2010). "How honey kills bacteria". FASEB J. 24 (7): 2576–82. doi:10.1096/fj.09-150789. PMID 20228250.
- ↑ "Sponge's secret weapon restores antibiotics' power". Science News.
- ↑ Suay I, Arenal F, Asensio FJ, Basilio A, Cabello MA, Díez MT, García JB, del Val AG, Gorrochategui J, Hernández P, Peláez F, Vicente MF (2000). "Screening of basidiomycetes for antimicrobial activities" (PDF). Antonie van Leeuwenhoek. 78 (2): 129–39. doi:10.1023/A:1026552024021. PMID 11204765.
- ↑ Appendino G, Gibbons S, Giana A, Pagani A, Grassi G, Stavri M, Smith E, Rahman MM (2008). "Antibacterial cannabinoids from Cannabis sativa: A structure-activity study". Journal of Natural Products. 71 (8): 1427–1430. doi:10.1021/np8002673. PMID 18681481.
- ↑ Russo EB (2011). "Taming THC: potential cannabis synergy and phytocannabinoid-terpenoid entourage effects". British Journal of Pharmacology. 163 (7): 1344–1364. doi:10.1111/j.1476-5381.2011.01238.x. PMC 3165946
 . PMID 21749363.
. PMID 21749363. - ↑ Appendino G, Gibbons S, Giana A, Pagani A, Grassi G, Stavri M, Smith E, Rahman MM (2008). "Antibacterial Cannabinoids from Cannabis sativa: A Structure-Activity Study". J. Nat. Prod. 71 (8): 1427–30. doi:10.1021/np8002673. PMID 18681481.
- ↑ Graham GS (2014). "Healing outcomes of MRSA-infected wounds with a protocol combining Oakin dressing with elements of the de-escalation theory". J Wound Care. 23 (2): S4, S6–8, S10–1. PMID 24600754.
- ↑ Thompson, Nick; Smith-Spark, Laura. "Thousand-year-old Anglo-Saxon potion kills MRSA superbug". CNN News. CNN/Time Warner. Retrieved 1 April 2015.
- ↑ Cutler RR, Wilson P (2004). "Antibacterial activity of a new, stable, aqueous extract of allicin against methicillin-resistant Staphylococcus aureus". Br J Biomed Sci. 52 (3): 71–74. PMID 15250668.
Further reading
There are several web-based resources available for further research and treatment options.
- The Center for Disease Control maintains MRSA pages that provide information surrounding the bacteria, including prevention, statistics, at risk groups, causes, educational resources, and environmental factors.
- The National Institute for Occupational Safety and Health maintains a webpage providing information on the bacteria, with respect to the workplace setting, and steps towards mitigating risk from MRSA infection.
- The National Institutes of Health maintains Medline Plus, a site for patients that provides information surrounding diseases, their causes, and treatments. Their MRSA pages provide research and information surrounding causes and treatment options.
- The Mayo Clinic maintains an online site, updated by Mayo Clinic staff, that covers the basic definition, symptoms, and patient education for MRSA.
- The online medical resource site, WebMD, maintains on MRSA that provide basic information about the bacteria, as well as some multimedia resources for patient education.
- MRSA MD is an online medical site devoted solely to MRSA education, treatment, and prevention. Maintained by Dr. Kirk Bortel, MRSA MD provides treatment information and prevention education.
- Maryn McKenna (2011). Superbug: The Fatal Menace of MRSA. Free Press. ISBN 978-1-4165-5728-9.