Gabapentin
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Neurontin, others[1] |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a694007 |
| License data | |
| Pregnancy category | |
| Routes of administration | By mouth |
| ATC code | N03AX12 (WHO) |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 27–60% (inversely proportional to dose; a high fat meal also increases bioavailability)[2][3] |
| Protein binding | Less than 3%[2][3] |
| Metabolism | Not significantly metabolised[2][3] |
| Biological half-life | 5 to 7 hours[2][3] |
| Excretion | Renal[2][3] |
| Identifiers | |
| |
| CAS Number |
60142-96-3 |
| PubChem (CID) | 3446 |
| IUPHAR/BPS | 5483 |
| DrugBank |
DB00996 |
| ChemSpider |
3328 |
| UNII |
6CW7F3G59X |
| KEGG |
D00332 |
| ChEBI |
CHEBI:42797 |
| ChEMBL |
CHEMBL940 |
| PDB ligand ID | GBN (PDBe, RCSB PDB) |
| ECHA InfoCard | 100.056.415 |
| Chemical and physical data | |
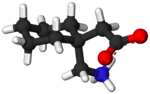
| Formula | C9H17NO2 |
| Molar mass | 171.237 g/mol |
| 3D model (Jmol) | Interactive image |
| |
| |
| (verify) | |
Gabapentin (GPN) marketed under the brand name Neurontin among others, is a medication used to treat epilepsy, neuropathic pain, hot flashes, and restless leg syndrome.[4][5] In epilepsy it may be used for those with partial seizures.[4] It is recommended as one of a number of first line medications for the treatment of neuropathic pain in diabetic neuropathy, post-herpetic neuralgia, and central neuropathic pain.[6] A 2014 review of its use for diabetic neuropathy and postherpetic neuralgia found about 14% of people have a meaningful benefit.[7]
Common side effects include sleepiness and dizziness. Serious side effects may include an increased risk of suicide, aggressive behaviour, and drug reaction with eosinophilia and systemic symptoms.[4] It is unclear if it is safe during pregnancy or breastfeeding.[8] Lower doses should be used in people with kidney problems. Gabapentin affects the inhibitory neurotransmitter γ-aminobutyric acid (GABA) but how it works is otherwise unclear.[4]
Gabapentin was first approved for use in 1993.[9] The wholesale price in the developing world is about US$40.50 per month.[10] In the United States it has been available as a generic medication since 2004.[4] As of 2015 the cost for a typical month of medication in the United States is US$100 to US$200.[11] During the 1990s Parke-Davis, a sub-company of Pfizer, used a number of techniques to encourage physicians in the United States to use gabapentin for unapproved uses.[12]
Medical uses
Gabapentin is used primarily to treat seizures and neuropathic pain.[13] It is also commonly prescribed for many off-label uses, such as treatment of anxiety disorders,[14][15] insomnia, and bipolar disorder.[14] There are, however, concerns regarding the quality of the trials conducted and evidence for some such uses, especially in the case of its use as a mood stabilizer in bipolar disorder.[16]
Seizures
Gabapentin is approved for treatment of focal seizures,[17] partial seizures and mixed seizures. There is insufficient evidence for its use in generalized epilepsy.[18]
Pain
A 2010 European Federation of Neurological Societies task force clinical guideline based on available evidence recommended gabapentin as a first-line treatment for diabetic neuropathy and postherpetic neuralgia with its highest level of evidence; it also recommended gabapentin as a first-line treatment for central pain but with lower evidence. It also found good evidence that a combination of gabapentin and morphine or oxycodone or nortriptyline worked better than either drug alone; the combination of gabapentin and venlafaxine may be better than gabapentin alone.[6]
A Cochrane review published in 2014 found that evidence of moderate quality shows that gabapentin can reduce pain by 50% for some people with postherpetic neuralgia (34% of people taking gabapentin in clinical trials versus 21% taking placebo) and for some people with painful diabetic neuropathy (38% versus 21%) and that there was not sufficient evidence to draw conclusions about other pain conditions; it also found no difference among various formulations or doses of gabapentin.[7]
A 2010 review found that it may be helpful in neuropathic pain due to cancer.[19] It is not effective in HIV-associated sensory neuropathy[20] and does not appear to provide benefit for complex regional pain syndrome.[21]
A 2009 review found gabapentin may reduce opioid use following surgery, but does not help with chronic pain after surgery.[22] A 2016 review found it does not help with pain following a knee replacement.[23]
It appears to be as effective as pregabalin and costs less.[24]
Migraine
The American Headache Society (AHS) and American Academy of Neurology (AAN) guidelines classify gabapentin as a drug with "insufficient data to support or refute use for migraine prophylaxis."[25] Furthermore, a 2013 Cochrane review concluded that gabapentin was not useful for the prevention of episodic migraine in adults.[26] Some have suggested that gabapentin may be effective for chronic migraine.[27]
Anxiety disorders
Gabapentin is effective in social anxiety disorder, panic disorder,[28][29] and generalized anxiety disorder.[14][15]
Other uses
Gabapentin may be useful in the treatment of comorbid anxiety in bipolar patients, (however not the bipolar state itself).[16][30][31] Gabapentin may be effective in acquired pendular nystagmus and infantile nystagmus, (but not periodic alternating nystagmus).[32][33] It is effective in hot flashes.[34][35][36] It may be effective in reducing pain and spasticity in multiple sclerosis.[37] Gabapentin may reduce symptoms of alcohol withdrawal (but it does not prevent the associated seizures).[38] Use for smoking cessation has had mixed results.[39][40] Gabapentin is effective in alleviating itching in kidney failure (uremic pruritus)[41] and itching of other causes.[42] It is an established treatment of restless leg syndrome.[43] Gabapentin may help sleeping problems in people with restless leg syndrome and partial seizures.[44][45] Gabapentin may be an option in essential or orthostatic tremor.[46][47][48]
Gabapentin is not effective alone as a mood-stabilizing treatment for bipolar disorder.[14] There is insufficient evidence to support its use in obsessive-compulsive disorder and treatment-resistant depression. Gabapentin does not appear effective for the treatment of tinnitus.[49]
Adverse effects
The most common side effects of gabapentin include dizziness, fatigue, drowsiness, ataxia, peripheral edema (swelling of extremities), nystagmus, and tremor.[50] Gabapentin may also produce sexual dysfunction in some patients, symptoms of which may include loss of libido, inability to reach orgasm, and erectile dysfunction.[51][52] Gabapentin should be used carefully in patients with renal impairment due to possible accumulation and toxicity.[53]
An increase in formation of adenocarcinomas was observed in rats during preclinical trials; however, the clinical significance of these results remains undetermined. Gabapentin is also known to induce pancreatic acinar cell carcinomas in rats through an unknown mechanism, perhaps by stimulation of DNA synthesis; these tumors did not affect the lifespan of the rats and did not metastasize.[54]
Suicide
In 2009 the U.S. Food and Drug Administration issued a warning of an increased risk of depression and suicidal thoughts and behaviors in patients taking gabapentin, along with other anticonvulsant drugs[55] modifying the packaging insert to reflect this.[50] A 2010 meta analysis confirmed the increased risk of suicide associated with gabapentin use.[56]
Overdose
Persons who accidentally or intentionally ingested overdoses may have drowsiness, sedation, blurred vision, slurred speech, somnolence and possibly death, if a very high amount was taken, particularly if combined with alcohol. Serum gabapentin concentrations may be measured to confirm diagnosis.[57]
Pharmacology
Gabapentin was initially synthesized to mimic the chemical structure of the neurotransmitter gamma-aminobutyric acid (GABA), but is believed to act on different brain receptors.
Some of its activity may involve interaction with voltage-gated calcium channels. Gabapentin binds to the α2δ subunit (1 and 2) and has been found to reduce calcium currents after chronic but not acute application via an effect on trafficking[58] of voltage-dependent calcium channels in the central nervous system.[59] Another possible mechanism of action is that gabapentin halts the formation of new synapses.[60]
Mechanism of action
The mechanism of the anticonvulsant action of gabapentin has not been fully described. Several possible mechanisms for pain improvement have been discussed.[61] Though similar in structure to the endogenous neurotransmitter GABA, gabapentin has not been shown to bind to GABA receptors at concentrations at or below 1 mM.[62] Gabapentin modulates the action of glutamate decarboxylase (GAD) and branched chain aminotransferase (BCAT), two enzymes involved in GABA biosynthesis. In human and rat studies, gabapentin was found to increase GABA biosynthesis, and to increase non-synaptic GABA neurotransmission in vitro.[63]
Gabapentin has been shown to bind to the α2δ-1 subunit of voltage gated calcium ion channels, which contributes to its pain attenuation effects in diabetic neuropathy and post-herpetic neuralgia. Other neurophysiological findings indicate that gabapentin also interacts with NMDA receptors, protein kinase C, and inflammatory cytokines.[62][64]
Society and culture
Sales
Gabapentin is best known under the brand name Neurontin manufactured by Pfizer subsidiary Parke-Davis. A Pfizer subsidiary named Greenstone markets generic gabapentin.
In December 2004 the FDA granted final approval to a generic equivalent to Neurontin made by the Israeli firm Teva.
Neurontin began as one of Pfizer's best selling drugs; however, Pfizer was criticized and under litigation for its marketing of the drug. They faced allegations that Parke-Davis marketed the drug for at least a dozen supposed uses that the FDA had not approved.[12][65] It has been used as a mainstay drug for migraines, even though it was not approved for such use in 2004.[66]
FDA approval
Gabapentin was originally approved by the U.S. Food and Drug Administration (FDA) in December 1993, for use as an adjuvant (effective when added to other antiseizure drugs) medication to control partial seizures in adults; that indication was extended to children in 2000.[67] In 2004, its use for treating postherpetic neuralgia (neuropathic pain following shingles) was approved.[67][68]
Off-label promotion
Although some small, non-controlled studies in the 1990s—mostly sponsored by gabapentin's manufacturer—suggested that treatment for bipolar disorder with gabapentin may be promising,[37] the preponderance of evidence suggests that it is not effective.[69] Subsequent to the corporate acquisition of the original patent holder, the pharmaceutical company Pfizer admitted that there had been violations of FDA guidelines regarding the promotion of unproven off-label uses for gabapentin in the Franklin v. Pfizer case.
Reuters reported on March 25, 2010, that "Pfizer Inc violated federal racketeering law by improperly promoting the epilepsy drug Neurontin ... Under federal RICO law the penalty is automatically tripled, so the finding will cost Pfizer $141 million."[70] The case stems from a claim from Kaiser Foundation Health Plan Inc. that "it was misled into believing Neurontin was effective for off-label treatment of migraines, bipolar disorder and other conditions. Pfizer argued that Kaiser physicians still recommend the drug for those uses."[71]
Bloomberg News reported "during the trial, Pfizer argued that Kaiser doctors continued to prescribe the drug even after the health insurer sued Pfizer in 2005. The insurer's website also still lists Neurontin as a drug for neuropathic pain, Pfizer lawyers said in closing argument."[72]
The Wall Street Journal noted that Pfizer spokesman Christopher Loder said, "We are disappointed with the verdict and will pursue post-trial motions and an appeal."[73] He would later add that "the verdict and the judge's rulings are not consistent with the facts and the law."[70]
Franklin v. Pfizer case
According to the San Francisco Chronicle, off-label prescriptions accounted for roughly 90 percent of Neurontin sales.[74]
While off-label prescriptions are common for a number of drugs and are legal, marketing of off-label uses of a drug is not.[12] In 2004, Warner-Lambert (which subsequently was acquired by Pfizer) agreed to plead guilty for activities of its Parke-Davis subsidiary, and to pay $430 million in fines to settle civil and criminal charges regarding the marketing of Neurontin for off-label purposes. The 2004 settlement was one of the largest in U.S. history, and the first off-label promotion case brought successfully under the False Claims Act.
Brand names
Gabapentin was originally marketed under the brand name Neurontin and since it became generic, it has been marketed under many other brand names.[1]

Related drugs
Parke-Davis developed a drug called pregabalin as a successor to gabapentin.[75] Pregabalin was brought to market by Pfizer as Lyrica after the company acquired Warner-Lambert. Pregabalin is related in structure to gabapentin.[76] Another new drug atagabalin has been trialed by Pfizer as a treatment for insomnia.[77]
A prodrug form (gabapentin enacarbil)[78] was approved in 2011 for the treatment of moderate-to-severe restless legs syndrome[79] and in 2012 for postherpetic neuralgia in adults.[80] It was designed for increased oral bioavailability over gabapentin.[81][82]
Veterinary use
Gabapentin is also used for some animal treatments, but some formulations (especially liquid forms) for human use contains the sweetener xylitol, which is toxic to dogs.[83]
References
- 1 2 Drugs.com international listings for Gabapentin Page accessed Feb. 9, 2016
- 1 2 3 4 5 "Neurontin, Gralise (gabapentin) dosing, indications, interactions, adverse effects, and more". Medscape Reference. WebMD. Retrieved 6 April 2014.
- 1 2 3 4 5 Goa, KL; Sorkin, EM (September 1993). "Gabapentin. A review of its pharmacological properties and clinical potential in epilepsy.". Drugs. 46 (3): 409–27. doi:10.2165/00003495-199346030-00007. PMID 7693432.
- 1 2 3 4 5 "Gabapentin". The American Society of Health-System Pharmacists. Retrieved Oct 23, 2015.
- ↑ Wijemanne, S; Jankovic, J (June 2015). "Restless legs syndrome: clinical presentation diagnosis and treatment.". Sleep medicine. 16 (6): 678–90. doi:10.1016/j.sleep.2015.03.002. PMID 25979181.
- 1 2 Attal N, Cruccu G, Baron R, et al. (September 2010). "EFNS guidelines on the pharmacological treatment of neuropathic pain: 2010 revision". Eur. J. Neurol. 17 (9): 1113–e88. doi:10.1111/j.1468-1331.2010.02999.x. PMID 20402746.
- 1 2 Moore, RA; Wiffen, PJ; Derry, S; Toelle, T; Rice, AS (27 April 2014). "Gabapentin for chronic neuropathic pain and fibromyalgia in adults.". The Cochrane database of systematic reviews. 4: CD007938. doi:10.1002/14651858.CD007938.pub3. PMID 24771480.
- ↑ "Gabapentin Pregnancy and Breastfeeding Warnings". Retrieved 13 March 2016.
- ↑ Pitkänen, Asla; Schwartzkroin, Philip A.; Moshé, Solomon L. (2005). Models of Seizures and Epilepsy. Burlington: Elsevier. p. 539. ISBN 9780080457024.
- ↑ "Gabapentin". International Drug Price Indicator Guide. Retrieved 13 March 2016.
- ↑ Hamilton, Richart (2015). Tarascon Pocket Pharmacopoeia 2015 Deluxe Lab-Coat Edition. Jones & Bartlett Learning. p. 327. ISBN 9781284057560.
- 1 2 3 Henney JE (August 2006). "Safeguarding patient welfare: who's in charge?" (PDF). Annals of Internal Medicine. 145 (4): 305–7. doi:10.7326/0003-4819-145-4-200608150-00013. PMID 16908923.
- ↑ "Gabapentin". The American Society of Health-System Pharmacists. Retrieved 3 April 2011.
- 1 2 3 4 Stephen V. Sobel (5 November 2012). Successful Psychopharmacology: Evidence-Based Treatment Solutions for Achieving Remission. W. W. Norton. p. 124. ISBN 978-0-393-70857-8.
- 1 2 D. John Reynolds; Jamie Coleman; Jeffrey Aronson (10 November 2011). Oxford Handbook of Practical Drug Therapy. Oxford University Press. p. 765. ISBN 978-0-19-956285-5.
- 1 2 Vedula, SS; Bero L; Scherer RW; Dickersin K (November 2009). "Outcome reporting in industry-sponsored trials of gabapentin for off-label use". The New England Journal of Medicine. 361 (20): 1963–71. doi:10.1056/NEJMsa0906126. PMID 19907043.
- ↑ Johannessen, SI; Ben-Menachem E (2006). "Management of focal-onset seizures: an update on drug treatment". Drugs. 66 (13): 1701–25. doi:10.2165/00003495-200666130-00004. PMID 16978035.
- ↑ French JA, Kanner AM, Bautista J, Abou-Khalil B, Browne T, Harden CL, Theodore WH, Bazil C, Stern J, Schachter SC, Bergen D, Hirtz D, Montouris GD, Nespeca M, Gidal B, Marks WJ, Turk WR, Fischer JH, Bourgeois B, Wilner A, Faught RE, Sachdeo RC, Beydoun A, Glauser TA (May 2004). "Efficacy and tolerability of the new antiepileptic drugs, I: Treatment of new-onset epilepsy: report of the TTA and QSS Subcommittees of the American Academy of Neurology and the American Epilepsy Society". Epilepsia. 45 (5): 401–9. doi:10.1111/j.0013-9580.2004.06204.x. PMID 15101821.
- ↑ Bar Ad, V (September 2010). "Gabapentin for the treatment of cancer-related pain syndromes". Reviews on Recent Clinical Trials. 5 (3): 174–8. doi:10.2174/157488710792007310. PMID 20482492.
- ↑ Phillips, TJ; Cherry CL; Cox S; Marshall SJ; Rice AS (2010-12-28). Pai, Nitika Pant, ed. "Pharmacological treatment of painful HIV-associated sensory neuropathy: a systematic review and meta-analysis of randomised controlled trials". Plos One. 5 (12): e14433. Bibcode:2010PLoSO...514433P. doi:10.1371/journal.pone.0014433. PMC 3010990
 . PMID 21203440.
. PMID 21203440. - ↑ Tran de, QH; Duong S; Bertini P; Finlayson RJ (February 2010). "Treatment of complex regional pain syndrome: a review of the evidence". Can J Anaesth. 57 (57(2)): 149–66. doi:10.1007/s12630-009-9237-0. PMID 20054678.
- ↑ Dauri, M; Faria, S; Gatti, A; Celidonio, L; Carpenedo, R; Sabato, AF (Aug 2009). "Gabapentin and pregabalin for the acute post-operative pain management. A systematic-narrative review of the recent clinical evidences.". Current drug targets. 10 (8): 716–33. doi:10.2174/138945009788982513. PMID 19702520.
- ↑ Hamilton, TW; Strickland, LH; Pandit, HG (17 August 2016). "A Meta-Analysis on the Use of Gabapentinoids for the Treatment of Acute Postoperative Pain Following Total Knee Arthroplasty.". The Journal of bone and joint surgery. American volume. 98 (16): 1340–50. PMID 27535436.
- ↑ Finnerup, NB; Sindrup SH; Jensen TS (September 2010). "The evidence for pharmacological treatment of neuropathic pain". Pain. 150 (3): 573–81. doi:10.1016/j.pain.2010.06.019. PMID 20705215.
- ↑ Loder, Elizabeth; Burch, Rebecca; Rizzoli, Paul (June 2012). "The 2012 AHS/AAN Guidelines for Prevention of Episodic Migraine: A Summary and Comparison With Other Recent Clinical Practice Guidelines" (PDF). Headache: The Journal of Head and Face Pain. 52 (6): 930–945. doi:10.1111/j.1526-4610.2012.02185.x. Retrieved 4 December 2016.
- ↑ Linde, M; Mulleners, WM; Chronicle, EP; McCrory, DC (Jun 24, 2013). "Gabapentin or pregabalin for the prophylaxis of episodic migraine in adults.". The Cochrane database of systematic reviews. 6: CD010609. doi:10.1002/14651858.CD010609. PMID 23797675.
- ↑ Diener, Hans-Christoph (2016). "Drug Treatment for Chronic Migraine.". Pharmacological Management of Headaches. Springer International Publishing. pp. 81–87.
- ↑ Mula M, Pini S, Cassano GB (June 2007). "The role of anticonvulsant drugs in anxiety disorders: a critical review of the evidence". J Clin Psychopharmacol. 27 (3): 263–72. doi:10.1097/jcp.0b013e318059361a. PMID 17502773.
- ↑ Alan F. Schatzberg; Jonathan O. Cole; Charles DeBattista (2010). Manual of Clinical Psychopharmacology. American Psychiatric Pub. pp. 344–345. ISBN 978-1-58562-377-8.
- ↑ Joseph F. Goldberg; Martin Harrow (1999). Bipolar Disorders: Clinical Course and Outcome. American Psychiatric Pub. p. 98. ISBN 978-0-88048-768-9.
- ↑ Freeman MP, Freeman SA, McElroy SL (February 2002). "The comorbidity of bipolar and anxiety disorders: prevalence, psychobiology, and treatment issues". J Affect Disord. 68 (1): 1–23. doi:10.1016/s0165-0327(00)00299-8. PMID 11869778.
- ↑ McLean, RJ; Gottlob I (August 2009). "The pharmacological treatment of nystagmus: a review". Expert opinion on pharmacotherapy. 10 (11): 1805–16. doi:10.1517/14656560902978446. PMID 19601699.
- ↑ Strupp, M; Brandt T (July 2009). "Current treatment of vestibular, ocular motor disorders and nystagmus". Therapeutic Advances in Neurological Disorders. 2 (4): 223–39. doi:10.1177/1756285609103120. PMC 3002631
 . PMID 21179531.
. PMID 21179531. - ↑ Toulis, KA; Tzellos T; Kouvelas D; Goulis DG (February 2009). "Gabapentin for the treatment of hot flashes in women with natural or tamoxifen-induced menopause: a systematic review and meta-analysis". Clinical therapeutics. 31 (2): 221–35. doi:10.1016/j.clinthera.2009.02.006. PMID 19302896.
- ↑ Cheema, D; Coomarasamy A; El-Toukhy T (November 2007). "Non-hormonal therapy of post-menopausal vasomotor symptoms: a structured evidence-based review". Archives of Gynecology and Obstetrics. 276 (5): 463–9. doi:10.1007/s00404-007-0390-9. PMID 17593379.
- ↑ Rada, G; Capurro, D; Pantoja, T; Corbalán, J; Moreno, G; Letelier, LM; Vera, C (Sep 8, 2010). "Non-hormonal interventions for hot flushes in women with a history of breast cancer.". The Cochrane database of systematic reviews (9): CD004923. doi:10.1002/14651858.CD004923.pub2. PMID 20824841.
- 1 2 Mack, Alicia (2003). "Examination of the evidence for off-label use of gabapentin" (PDF). Journal of Managed Care Pharmacy. 9 (6): 559–68. PMID 14664664.
- ↑ Muncie HL, Jr; Yasinian, Y; Oge', L (Nov 1, 2013). "Outpatient management of alcohol withdrawal syndrome.". American family physician. 88 (9): 589–95. PMID 24364635.
- ↑ Sood, A; Ebbert JO; Schroeder DR; Croghan IT; Sood R; Vander Weg MW; Wong GY; Hays JT (February 2007). "Gabapentin for smoking cessation: a preliminary investigation of efficacy". Nicotine & Tobacco Research. 9 (2): 291–8. doi:10.1080/14622200601080307. PMID 17365760.
- ↑ Sood, A; Ebbert JO; Wyatt KD; Croghan IT; Schroeder DR; Sood R; Hays JT (March 2010). "Gabapentin for smoking cessation". Nicotine & Tobacco Research. 12 (3): 300–4. doi:10.1093/ntr/ntp195. PMC 2825098
 . PMID 20081039.
. PMID 20081039. - ↑ Berger, TG; Steinhoff, M (June 2011). "Pruritus and renal failure.". Seminars in cutaneous medicine and surgery. 30 (2): 99–100. doi:10.1016/j.sder.2011.04.005. PMID 21767770.
- ↑ Anand S (March 2013). "Gabapentin for pruritus in palliative care". American Journal of Hospice and Palliative Medicine. 30 (2): 192–196. doi:10.1177/1049909112445464.
- ↑ Scott LJ (December 2012). "Gabapentin enacarbil: in patients with restless legs syndrome". CNS Drugs. 26 (12): 1073–83. doi:10.1007/s40263-012-0020-3. PMID 23179641.
- ↑ Jack D. Edinger (2013). Insomnia, an Issue of Sleep Medicine Clinics. Elsevier Health Sciences. p. 339. ISBN 978-0-323-18872-2.
- ↑ Charles M. Morin; Colin A. Espie (2 February 2012). The Oxford Handbook of Sleep and Sleep Disorders. Oxford University Press. p. 544. ISBN 978-0-19-970442-2.
- ↑ Schneider SA, Deusch G (January 2014). "The treatment of tremor". Neurotherapeutics. 11 (1): 128–138. doi:10.1007/s13311-013-0230-5. PMC 3899476
 . PMID 24142589.
. PMID 24142589. - ↑ Zesiewicz TA; et al. (November 2011). "Evidence-based guideline update: treatment of essential tremor: report of the Quality Standards subcommittee of the American Academy of Neurology". Neurology. 77 (19): 1752–1755. doi:10.1212/WNL.0b013e318236f0fd. PMC 3208950
 . PMID 22013182.
. PMID 22013182. - ↑ Sadeghi R, Ondo WG (December 2010). "Pharmacological management of essential tremor". Drugs. 70 (17): 2215–2228. doi:10.2165/11538180-000000000-00000. PMID 21080739.
- ↑ Aazh, H; El Refaie, A; Humphriss, R (December 2011). "Gabapentin for tinnitus: a systematic review.". American Journal of Audiology. 20 (2): 151–8. doi:10.1044/1059-0889(2011/10-0041). PMID 21940981.
- 1 2 "Neurontin packaging insert" (pdf). U.S. Food and Drug Administration (FDA). 2009-05-01. Retrieved 2010-07-16.
- ↑ Jeffrey K Aronson (4 March 2014). Side Effects of Drugs Annual: A worldwide yearly survey of new data in adverse drug reactions. Newnes. p. 137. ISBN 978-0-444-62636-3.
- ↑ American Psychiatric Association. The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition.: DSM 5. bookpointUS. p. 482. GGKEY:LXJWL7ZHDAH.
- ↑ "www.accessdata.fda.gov" (PDF).
- ↑ Gabapentin Official FDA information, side effects and uses
- ↑ "Suicidal Behavior and Ideation and Antiepileptic Drugs". U.S. Food and Drug Administration (FDA).
- ↑ Patorno E, Bohn RL, Wahl PM, et al. (April 2010). "Anticonvulsant medications and the risk of suicide, attempted suicide, or violent death". JAMA. 303 (14): 1401–9. doi:10.1001/jama.2010.410. PMID 20388896.
- ↑ R.C. Baselt, Disposition of Toxic Drugs and Chemicals in Man, 8th edition, Biomedical Publications, Foster City, CA, 2008, pp. 677–8. ISBN 978-0-9626523-7-0.
- ↑ Hendrich, J; Van Minh, AT; Heblich, F; Nieto-Rostro, M; Watschinger, K; Striessnig, J; Wratten, J; Davies, A; Dolphin, AC (March 2008). "Pharmacological disruption of calcium channel trafficking by the alpha2delta ligand gabapentin" (PDF). Proceedings of the National Academy of Sciences of the United States of America. 105 (9): 3628–33. Bibcode:2008PNAS..105.3628H. doi:10.1073/pnas.0708930105. PMC 2265195
 . PMID 18299583.
. PMID 18299583. - ↑ Davies, A; Hendrich, J; Van Minh, AT; Wratten, J; Douglas, L; Dolphin, AC (May 2007). "Functional biology of the alpha(2)delta subunits of voltage-gated calcium channels". Trends Pharmacol Sci. 28 (5): 220–8. doi:10.1016/j.tips.2007.03.005. PMID 17403543.
- ↑ Eroglu, Ç; Allen, NJ; Susman, MW; O'Rourke, NA; Park, CY; Özkan, E; Chakraborty, C; Mulinyawe, SB; et al. (October 2009). "The Gabapentin Receptor α2δ-1 is the Neuronal Thrombospondin Receptor Responsible for Excitatory CNS Synaptogenesis". Cell. 139 (2): 380–92. doi:10.1016/j.cell.2009.09.025. PMC 2791798
 . PMID 19818485.
. PMID 19818485. - ↑ "Mechanisms of the gabapentinoids and α2δ-1 calcium channel subunit in neuropathic pain". Pharmacology research and perspectives. 4. 2016. doi:10.1002/prp2.205.
- 1 2 "Product Monograph". Pfizer. Retrieved 28 September 2014.
- ↑ Taylor, CP (1997). "Mechanisms of action of gabapentin". Rev. Neurol. (Paris). 153 Suppl 1: S39–45. PMID 9686247.
- ↑ Kukkar Ankesh. "Implications and mechanism of action of gabapentin in neuropathic pain". Archives of Pharmacal Research. 36: 237–251. doi:10.1007/s12272-013-0057-y.
- ↑ "Warner–Lambert to pay $430 million to resolve criminal & civil health care liability relating to off-label promotion" (Press release). Department of Justice. May 13, 2004. Retrieved December 2, 2009.
- ↑ Mathew, NT; Rapoport, A; Saper, J; Magnus, L; Klapper, J; Ramadan, N; Stacey, B; Tepper, S (February 2001). "Efficacy of Gabapentin in Migraine Prophylaxis". Headache: the Journal of Head and Face Pain. 41 (2): 119–28. doi:10.1046/j.1526-4610.2001.111006119.x. PMID 11251695.
- 1 2 Mack A (2003). "Examination of the evidence for off-label use of gabapentin" (PDF). J Manag Care Pharm. 9 (6): 559–68. PMID 14664664.
- ↑ Pfizer Neurontin Label, Revised: 5/2013 Retrieved 9 August 2014
- ↑ Reinares M, Rosa AR, Franco C, et al. (March 2013). "A systematic review on the role of anticonvulsants in the treatment of acute bipolar depression". Int. J. Neuropsychopharmacol. 16 (2): 485–96. doi:10.1017/S1461145712000491. PMID 22575611.
- 1 2 Berkrot, Bill (2010-03-25). "US jury's Neurontin ruling to cost Pfizer $141 mln". Reuters.
- ↑ "Pfizer faces $142M in damages for drug fraud". Business Week. 2010-03-25. Retrieved 13 January 2012.
- ↑ Bob Van Voris; Janelle Lawrence (2010-03-26). "Pfizer Told to Pay $142.1 Million for Neurontin Marketing Fraud". Bloomberg News. Retrieved 13 January 2012.
- ↑ Jon Kamp (2010-03-25). "Jury Rules Against Pfizer in Marketing Case". The Wall Street Journal. Retrieved 13 January 2012.
- ↑ Tansey, Bernadette (2004-05-14). "Huge penalty in drug fraud, Pfizer settles felony case in Neurontin off-label promotion". San Francisco Chronicle. p. C-1.
- ↑ Baillie, JK; Power, I (January 2006). "The mechanism of action of gabapentin in neuropathic pain". Curr Opin Investig Drugs. 7 (1): 33–9. ISSN 1472-4472. PMID 16425669.
- ↑ Jensen B, Regier LD, editors. RxFiles : Drug comparison charts. 7th ed. Saskatoon, SK: RxFiles, 2010; p.78
- ↑ Kjellsson MC, Ouellet D, Corrigan B, Karlsson MO (June 2011). "Modeling Sleep Data for a New Drug in Development using Markov Mixed-Effects Models". Pharmaceutical Research. 28 (10): 2610–27. doi:10.1007/s11095-011-0490-x. PMID 21681607.
- ↑ Landmark CJ, Johannessen SI (2008). "Modifications of antiepileptic drugs for improved tolerability and efficacy". Perspectives in Medicinal Chemistry. 2: 21–39. PMC 2746576
 . PMID 19787095.
. PMID 19787095. - ↑
- ↑ Jeffrey, Susan. "FDA Approves Gabapentin Enacarbil for Postherpetic Neuralgia". Medscape.
- ↑ Cundy KC, Branch R, Chernov-Rogan T, Dias T, Estrada T, Hold K, Koller K, Liu X, Mann A, Panuwat M, Raillard SP, Upadhyay S, Wu QQ, Xiang JN, Yan H, Zerangue N, Zhou CX, Barrett RW, Gallop MA (October 2004). "XP13512 [(+/-)-1-([(alpha-isobutanoyloxyethoxy)carbonyl] aminomethyl)-1-cyclohexane acetic acid], a novel gabapentin prodrug: I. Design, synthesis, enzymatic conversion to gabapentin, and transport by intestinal solute transporters". The Journal of Pharmacology and Experimental Therapeutics. 311 (1): 315–23. doi:10.1124/jpet.104.067934. PMID 15146028.
- ↑ Cundy KC, Annamalai T, Bu L, De Vera J, Estrela J, Luo W, Shirsat P, Torneros A, Yao F, Zou J, Barrett RW, Gallop MA (October 2004). "XP13512 [(+/-)-1-([(alpha-isobutanoyloxyethoxy)carbonyl] aminomethyl)-1-cyclohexane acetic acid], a novel gabapentin prodrug: II. Improved oral bioavailability, dose proportionality, and colonic absorption compared with gabapentin in rats and monkeys". The Journal of Pharmacology and Experimental Therapeutics. 311 (1): 324–33. doi:10.1124/jpet.104.067959. PMID 15146029.
- ↑ Barbara Forney. "Gabapentin for Veterinary Use".
External links
- DrugBank: gabapentin
- Gabapentin information from MedlinePlus
- "Gabapentin" PubMed Health. National Center for Biotechnology Information (NCBI)
- "Suicidal Behavior and Ideation and Antiepileptic Drugs" U.S. Food and Drug Administration (FDA)
- Neurontin collected news and commentary at The New York Times
- "Gabapentin" Drug Information Portal. U.S. National Library of Medicine.