Bispecific monoclonal antibody
A bispecific monoclonal antibody (BsMAb, BsAb) is an artificial protein that is composed of fragments of two different monoclonal antibodies and consequently binds to two different types of antigen. The most widely used application of this approach is in cancer immunotherapy, where BsMAbs are engineered that simultaneously bind to a cytotoxic cell (using a receptor like CD3) and a target like a tumour cell to be destroyed.[1][2]
Structural types

In order to overcome manufacturing difficulties, a first-generation BsMAb, called trifunctional antibody, has been developed. It consists of two heavy and two light chains, one each from two different antibodies. The two Fab regions (the arms) are directed against two antigens. The Fc region (the foot) is made up from the two heavy chains and forms the third binding site; hence the name.[1][2][3]
Other types of bispecific antibodies have been designed to overcome certain problems, such as short half-life, immunogenicity and side-effects caused by cytokine liberation. They include chemically linked Fabs, consisting only of the Fab regions, and various types of bivalent and trivalent single-chain variable fragments (scFvs), fusion proteins mimicking the variable domains of two antibodies. The furthest developed of these newer formats are the bi-specific T-cell engagers (BiTEs)[4] and mAb2's, antibodies engineered to contain an Fcab antigen-binding fragment instead of the Fc constant region.[5][6]
Mechanism of action
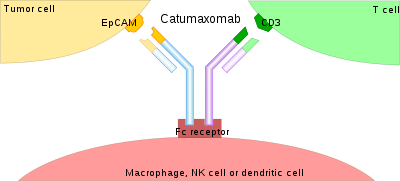
Of the two paratopes that form the tops of the variable domains, one can be directed against a tumour antigen and the other against a T-lymphocyte antigen like CD3. In the case of trifunctional antibodies, the Fc region additionally binds to a cell that expresses Fc receptors, like a macrophage, a natural killer cell or a dendritic cell. In sum, the tumour cell is connected to one or two cells of the immune system, which subsequently destroy it.[3][4]
Advantages over ordinary monoclonal antibodies
Cancer immunotherapy with ordinary monoclonal antibodies does not activate T-lymphocytes because this type of cell does not possess Fc receptors, so the Fc region cannot bind to them, and the Fab regions are already used for binding the tumour cells.[7] Bispecific antibodies have a higher cytotoxic potential. They bind to antigens that are expressed relatively weakly.[8] The effective dose is around 0.01 mg·m−2·d−1 (milligrams per square metre body surface area per day), several orders of magnitude lower than with ordinary antibodies.[7] Additionally, targeting more than one molecule can be useful to circumvent the regulation of parallel pathways and avoid the appearance of resistance to the treatment.[9]
References
![]() This article incorporates public domain material from the U.S. National Cancer Institute document "Dictionary of Cancer Terms".
This article incorporates public domain material from the U.S. National Cancer Institute document "Dictionary of Cancer Terms".
- 1 2 Mueller, D; Kontermann, RE (2010). "Bispecific antibodies for cancer immunotherapy". BioDrugs. 24 (2): 89–98. doi:10.2165/11530960-000000000-00000. PMID 20199124.
- 1 2 Chames, P; Baty, D (2009). "Bispecific antibodies for cancer therapy: The light at the end of the tunnel". MAbs. 1 (6): 539–547. doi:10.4161/mabs.1.6.10015. PMC 2791310
 . PMID 20073127.
. PMID 20073127. - 1 2 Lindhofer, H; Mocikat, R; Steipe, B; Thierfelder, S (1 July 1995). "Preferential species-restricted heavy/light chain pairing in rat/mouse quadromas. Implications for a single-step purification of bispecific antibodies". Journal of Immunology. Journal of Immunology. 155 (1): 219–25. PMID 7602098.
- 1 2 Baeuerle, PA; Reinhardt, C (2009). "Bispecific T-cell engaging antibodies for cancer therapy". Cancer Res. 69 (12): 4941–4944. doi:10.1158/0008-5472.CAN-09-0547. PMID 19509221.
- ↑ Wozniak-Knopp G, Bartl S, Bauer A, Mostageer M, Woisetschläger M, Antes B, Ettl K, Kainer M, Weberhofer G, Wiederkum S, Himmler G, Mudde GC, Rüker F (2010). "Introducing antigen-binding sites in structural loops of immunoglobulin constant domains: Fc fragments with engineered HER2/neu-binding sites and antibody properties.". Protein Eng Des. 23 (4): 289–297. doi:10.1093/protein/gzq005. PMID 20150180.
- ↑ http://www.f-star.com/bispecific-mAb2.php
- 1 2 Bargou, R; Leo, E; Zugmaier, G; Klinger, M; Goebeler, M; Knop, S; Noppeney, R; Viardot, A; et al. (2008). "Tumor regression in cancer patients by very low doses of a T cell-engaging antibody". Science. 321 (5891): 974–977. doi:10.1126/science.1158545. PMID 18703743.
- ↑ Weiner, LM; Holmes, M; Richeson, A; Godwin, A; Adams, GP; Hsieh-Ma, ST; Ring, DB; Alpaugh, RK (1993). "Binding and cytotoxicity characteristics of the bispecific murine monoclonal antibody 2B1". Journal of immunology (Baltimore, Md. : 1950). 151 (5): 2877–86. PMID 8103070.
- ↑ Varela, MA (2015). "Identification of sequences common to more than one therapeutic target to treat complex diseases: simulating the high variance in sequence interactivity evolved to modulate robust phenotypes". BMC Genomics. 16: 530. doi:10.1186/s12864-015-1727-6. PMID 26187740.
External links
- Bispecific monoclonal antibody entry in the public domain NCI Dictionary of Cancer Terms
- Bispecific antibodies at the US National Library of Medicine Medical Subject Headings (MeSH)