Anxiety disorder
| Anxiety disorder | |
|---|---|
|
| |
| Classification and external resources | |
| Specialty | Psychiatry |
| ICD-10 | F40-F42 |
| ICD-9-CM | 300 |
| DiseasesDB | 787 |
| eMedicine | med/152 |
| MeSH | D001008 |
Anxiety disorders are a group of mental disorders characterized by feelings of anxiety and fear.[2] Anxiety is a worry about future events and fear is a reaction to current events. These feelings may cause physical symptoms, such as a fast heart rate and shakiness. There are a number of anxiety disorders: including generalized anxiety disorder, specific phobia, social anxiety disorder, separation anxiety disorder, agoraphobia, and panic disorder. The disorder differs by what results in the symptoms. People often have more than one anxiety disorder.[2]
The cause of anxiety disorders is a combination of genetic and environmental factors.[3] Risk factors include a history of child abuse, family history of mental disorders, and poverty. Anxiety disorders often occur with other mental disorders, particularly major depressive disorder, personality disorder, and substance use disorder.[4] To be diagnosed symptoms typically need to be present at least six months, be more than would be expected for the situation, and decrease functioning.[2][4] Other problems that may result in similar symptoms including hyperthyroidism, heart disease, caffeine, alcohol, or cannabis use, and withdrawal from certain drugs, among others.[4][5]
Without treatment, anxiety disorders tend to remain.[2][3] Treatment may include lifestyle changes, counselling, and medications. Counselling is typically with a type of cognitive behavioural therapy.[4] Medications, such as antidepressants or beta blockers, may improve symptoms.[3]
About 12% of people are affected by an anxiety disorder in a given year and between 5-30% are affected at some point in their life.[4][6] They occur about twice as often in females as males, and generally begin before the age of 25.[2][4] The most common are specific phobia which affects nearly 12% and social anxiety disorder which affects 10% at some point in their life. They affect those between the ages of 15 and 35 the most and become less common after the age of 55. Rates appear to be higher in the United States and Europe.[4]
Classification
.jpg)
Generalized
Generalized anxiety disorder (GAD) is a common, chronic disorder characterized by long-lasting anxiety that is not focused on any one object or situation. Those suffering from generalized anxiety disorder experience non-specific persistent fear and worry, and become overly concerned with everyday matters. Generalized anxiety disorder is "characterized by chronic excessive worry accompanied by three or more of the following symptoms: restlessness, fatigue, concentration problems, irritability, muscle tension, and sleep disturbance".[7] Generalized anxiety disorder is the most common anxiety disorder to affect older adults.[8] Anxiety can be a symptom of a medical or substance abuse problem, and medical professionals must be aware of this. A diagnosis of GAD is made when a person has been excessively worried about an everyday problem for six months or more.[9] A person may find that they have problems making daily decisions and remembering commitments as a result of lack of concentration/preoccupation with worry.[10] Appearance looks strained, with increased sweating from the hands, feet, and axillae,[11] and they may be tearful, which can suggest depression.[12] Before a diagnosis of anxiety disorder is made, physicians must rule out drug-induced anxiety and other medical causes.[13]
In children GAD may be associated with headaches, restlessness, abdominal pain, and heart palpitations.[14] Typically it begins around 8 to 9 years of age.[14]
Phobias
The single largest category of anxiety disorders is that of phobic disorders, which includes all cases in which fear and anxiety are triggered by a specific stimulus or situation. Between 5% and 12% of the population worldwide suffer from phobic disorders.[9] Sufferers typically anticipate terrifying consequences from encountering the object of their fear, which can be anything from an animal to a location to a bodily fluid to a particular situation. Sufferers understand that their fear is not proportional to the actual potential danger but still are overwhelmed by it.[15]
Panic disorder
With panic disorder, a person has brief attacks of intense terror and apprehension, often marked by trembling, shaking, confusion, dizziness, nausea, and/or difficulty breathing. These panic attacks, defined by the APA as fear or discomfort that abruptly arises and peaks in less than ten minutes, can last for several hours.[16] Attacks can be triggered by stress, fear, or even exercise; the specific cause is not always apparent.
In addition to recurrent unexpected panic attacks, a diagnosis of panic disorder requires that said attacks have chronic consequences: either worry over the attacks' potential implications, persistent fear of future attacks, or significant changes in behavior related to the attacks. As such, those suffering from panic disorder experience symptoms even outside specific panic episodes. Often, normal changes in heartbeat are noticed by a panic sufferer, leading them to think something is wrong with their heart or they are about to have another panic attack. In some cases, a heightened awareness (hypervigilance) of body functioning occurs during panic attacks, wherein any perceived physiological change is interpreted as a possible life-threatening illness (i.e., extreme hypochondriasis).
Agoraphobia
Agoraphobia is the specific anxiety about being in a place or situation where escape is difficult or embarrassing or where help may be unavailable.[17] Agoraphobia is strongly linked with panic disorder and is often precipitated by the fear of having a panic attack. A common manifestation involves needing to be in constant view of a door or other escape route. In addition to the fears themselves, the term agoraphobia is often used to refer to avoidance behaviors that sufferers often develop.[18] For example, following a panic attack while driving, someone suffering from agoraphobia may develop anxiety over driving and will therefore avoid driving. These avoidance behaviors can often have serious consequences and often reinforce the fear they are caused by.
Social anxiety disorder
Social anxiety disorder (SAD; also known as social phobia) describes an intense fear and avoidance of negative public scrutiny, public embarrassment, humiliation, or social interaction. This fear can be specific to particular social situations (such as public speaking) or, more typically, is experienced in most (or all) social interactions. Social anxiety often manifests specific physical symptoms, including blushing, sweating, and difficulty speaking. As with all phobic disorders, those suffering from social anxiety often will attempt to avoid the source of their anxiety; in the case of social anxiety this is particularly problematic, and in severe cases can lead to complete social isolation.
Social physique anxiety (SPA) is a subtype of social anxiety. It is concern over the evaluation of one's body by others.[19] SPA is common among adolescents, especially females.
Post-traumatic stress disorder
Post-traumatic stress disorder (PTSD) is an anxiety disorder that results from a traumatic experience. Post-traumatic stress can result from an extreme situation, such as combat, natural disaster, rape, hostage situations, child abuse, bullying, or even a serious accident. It can also result from long-term (chronic) exposure to a severe stressor,[20] for example soldiers who endure individual battles but cannot cope with continuous combat. Common symptoms include hypervigilance, flashbacks, avoidant behaviors, anxiety, anger and depression.[21] There are a number of treatments that form the basis of the care plan for those suffering with PTSD. Such treatments include cognitive behavioral therapy (CBT), psychotherapy and support from family and friends.[9]
Posttraumatic stress disorder (PTSD) research began with Vietnam veterans, as well as natural and non natural disaster victims. Studies have found the degree of exposure to a disaster has been found to be the best predictor of PTSD.[22]
Separation anxiety
Separation anxiety disorder (SepAD) is the feeling of excessive and inappropriate levels of anxiety over being separated from a person or place. Separation anxiety is a normal part of development in babies or children, and it is only when this feeling is excessive or inappropriate that it can be considered a disorder.[23] Separation anxiety disorder affects roughly 7% of adults and 4% of children, but the childhood cases tend to be more severe; in some instances, even a brief separation can produce panic.[24][25] Treating a child earlier may prevent problems. This may include training the parents and family on how to deal with it. Often, the parents will reinforce the anxiety because they do not know how to properly work through it with the child. In addition to parent training and family therapy, medication, such as SSRI's, can be used to treat separation anxiety.[26]
Situational anxiety
Situational anxiety is caused by new situations or changing events. It can also be caused by various events that make that particular individual uncomfortable. Its occurrence is very common. Often, an individual will experience panic attacks or extreme anxiety in specific situations. A situation that causes one individual to experience anxiety may not affect another individual at all. For example, some people become uneasy in crowds or tight spaces, so standing in a tightly packed line, say at the bank or a store register, may cause them to experience extreme anxiety, possibly a panic attack.[27] Others, however, may experience anxiety when major changes in life occur, such as entering college, getting married, having children, etc.
Obsessive–compulsive disorder
Obsessive–compulsive disorder (OCD) is not classified as an anxiety disorder by the DSM-5 but is by the ICD-10. It was previously classified as an anxiety disorder in the DSM-4. It is a condition where the person has obsessions (distressing, persistent, and intrusive thoughts or images) and/or compulsions (urges to repeatedly perform specific acts or rituals), that are not caused by drugs or physical order, and which cause distress or social dysfunction.[28][29] The compulsive rituals are personal rules followed to relieve the anxiety.[29] OCD affects roughly 1-2% of adults (somewhat more women than men), and under 3% of children and adolescents.[28][29]
A person with OCD knows that the symptoms are unreasonable and struggles against both the thoughts and the behavior.[28][30] Their symptoms could be related to external events they fear (such as their home burning down because they forget to turn off the stove) or worry that they will behave inappropriately.[30]
It is not certain why some people have OCD, but behavioral, cognitive, genetic, and neurobiological factors may be involved.[29] Risk factors include family history, being single (although that may result from the disorder), and higher socioeconomic class or not being in paid employment.[29] OCD is chronic; about 20% of people will overcome it, and symptoms will at least reduce over time for most people (a further 50%).[28]
Causes
Drugs
Anxiety and depression can be caused by alcohol abuse, which in most cases improves with prolonged abstinence. Even moderate, sustained alcohol use may increase anxiety levels in some individuals.[31] Caffeine, alcohol and benzodiazepine dependence can worsen or cause anxiety and panic attacks.[32] Anxiety commonly occurs during the acute withdrawal phase of alcohol and can persist for up to 2 years as part of a post-acute withdrawal syndrome, in about a quarter of people recovering from alcoholism.[33] In one study in 1988–1990, illness in approximately half of patients attending mental health services at one British hospital psychiatric clinic, for conditions including anxiety disorders such as panic disorder or social phobia, was determined to be the result of alcohol or benzodiazepine dependence. In these patients, an initial increase in anxiety occurred during the withdrawal period followed by a cessation of their anxiety symptoms.[34]
There is evidence that chronic exposure to organic solvents in the work environment can be associated with anxiety disorders. Painting, varnishing and carpet-laying are some of the jobs in which significant exposure to organic solvents may occur.[35]
Taking caffeine may cause or worsen anxiety disorders,[36][37] including panic disorder.[38][39][40] Those with anxiety disorders can have high caffeine sensitivity.[41][42] Caffeine-induced anxiety disorder is a subclass of the DSM-5 diagnosis of substance/medication-induced anxiety disorder. Substance/medication-induced anxiety disorder falls under the category of anxiety disorders, and not the category of substance-related and addictive disorders, even though the symptoms are due to the effects of a substance.[43]
Cannabis use is associated with anxiety disorders. However, the precise relationship between cannabis use and anxiety still needs to be established.[44][45]
Medical conditions
Occasionally, an anxiety disorder may be a side-effect of an underlying endocrine disease that causes nervous system hyperactivity, such as pheochromocytoma[46][47] or hyperthyroidism.[48]
Stress
Anxiety disorders can arise in response to life stresses such as financial worries or chronic physical illness. Anxiety among adolescents and young adults is common due to the stresses of social interaction, evaluation, and body image. Anxiety is also common among older people who have dementia. On the other hand, anxiety disorder is sometimes misdiagnosed among older adults when doctors misinterpret symptoms of a physical ailment (for instance, racing heartbeat due to cardiac arrhythmia) as signs of anxiety.[8]
Genetics
GAD runs in families and is six times more common in the children of someone with the condition.[49]
While anxiety arose as an adaptation, in modern times it is almost always thought of negatively in the context of anxiety disorders. People with these disorders have highly sensitive systems; hence, their systems tend to overreact to seemingly harmless stimuli. Sometimes anxiety disorders occur in those who have had traumatic youths, demonstrating an increased prevalence of anxiety when it appears a child will have a difficult future.[50] In these cases, the disorder arises as a way to predict that the individual’s environment will continue to pose threats.
Persistence of anxiety
At a low level, anxiety is not a bad thing. In fact, the hormonal response to anxiety has evolved as a benefit, as it helps humans react to dangers. Researchers in evolutionary medicine believe this adaptation allows humans to realize there is a potential threat and to act accordingly in order to ensure greatest possibility of protection. It has actually been shown that those with low levels of anxiety have a greater risk of death than those with average levels. This is because the absence of fear can lead to injury or death.[50] Additionally, patients with both anxiety and depression were found to have lower morbidity than those with depression alone.[51] The functional significance of the symptoms associated with anxiety includes: greater alertness, quicker preparation for action, and reduced probability of missing threats.[51] In the wild, vulnerable individuals, for example those who are hurt or pregnant, have a lower threshold for anxiety response, making them more alert.[51] This demonstrates a lengthy evolutionary history of the anxiety response.
Evolutionary mismatch
It has been theorized that high rates of anxiety are a reaction to how the social environment has changed from the Paleolithic era. For example, in the Stone Age there was greater skin-to-skin contact and more handling of babies by their mothers, both of which are strategies that reduce anxiety.[50] Additionally, there is greater interaction with strangers in present times as opposed to interactions solely between close-knit tribes. Researchers posit that the lack of constant social interaction, especially in the formative years, is a driving cause of high rates of anxiety.
Many current cases are likely to have resulted from an evolutionary mismatch, which has been specifically termed a "psychopathogical mismatch." In evolutionary terms, a mismatch occurs when an individual possesses traits that were adapted for an environment that differs from the individual’s current environment. For example, even though an anxiety reaction may have been evolved to help with life-threatening situations, for highly sensitized individuals in Westernized cultures simply hearing bad news can elicit a strong reaction.[52]
An evolutionary perspective may provide insight into alternatives to current clinical treatment methods for anxiety disorders. Simply knowing some anxiety is beneficial may alleviate some of the panic associated with mild conditions. Some researchers believe that, in theory, anxiety can be mediated by reducing a patient’s feeling of vulnerability and then changing their appraisal of the situation.[52]
Mechanisms
Biological
Low levels of GABA, a neurotransmitter that reduces activity in the central nervous system, contribute to anxiety. A number of anxiolytics achieve their effect by modulating the GABA receptors.[53][54][55]
Selective serotonin reuptake inhibitors, the drugs most commonly used to treat depression, are frequently considered as a first line treatment for anxiety disorders.[56]
Amygdala
The amygdala is central to the processing of fear and anxiety, and its function may be disrupted in anxiety disorders.[57] Sensory information enters the amygdala through the nuclei of the basolateral complex (consisting of lateral, basal, and accessory basal nuclei). The basolateral complex processes sensory-related fear memories and communicates their threat importance to memory and sensory processing elsewhere in the brain, such as the medial prefrontal cortex and sensory cortices.
Another important area is the adjacent central nucleus of the amygdala, which controls species-specific fear responses, via connections to the brainstem, hypothalamus, and cerebellum areas. In those with general anxiety disorder, these connections functionally seem to be less distinct, with greater gray matter in the central nucleus. Another difference is that the amygdala areas have decreased connectivity with the insula and cingulate areas that control general stimulus salience, while having greater connectivity with the parietal cortex and prefrontal cortex circuits that underlie executive functions.[57]
The latter suggests a compensation strategy for dysfunctional amygdala processing of anxiety. Researchers have noted "Amygdalofrontoparietal coupling in generalized anxiety disorder patients may ... reflect the habitual engagement of a cognitive control system to regulate excessive anxiety."[57] This is consistent with cognitive theories that suggest the use in this disorder of attempts to reduce the involvement of emotions with compensatory cognitive strategies.
Clinical and animal studies suggest a correlation between anxiety disorders and difficulty in maintaining balance.[58][59][60][61] A possible mechanism is malfunction in the parabrachial area, a brain structure that, among other functions, coordinates signals from the amygdala with input concerning balance.[62]
Anxiety processing in the basolateral amygdala has been implicated with dendritic arborization of the amygdaloid neurons. SK2 potassium channels mediate inhibitory influence on action potentials and reduce arborization. By overexpressing SK2 in the basolateral amygdala, anxiety in experimental animals can be reduced together with general levels of stress-induced corticosterone secretion.[63]
Prevention
Focus is increasing on prevention of anxiety disorders.[64] There is tentative evidence to support the use of cognitive behavior therapy[64] and mindfulness therapy.[65][66] As of 2013, there are no effective measures to prevent GAD in adults.[67]
Diagnosis
Anxiety disorders are often severe chronic conditions, which can be present from an early age or begin suddenly after a triggering event. They are prone to flare up at times of high stress and are frequently accompanied by physiological symptoms such as headache, sweating, muscle spasms, tachycardia, palpitations, and hypertension, which in some cases lead to fatigue.
In casual discourse the words "anxiety" and "fear" are often used interchangeably; in clinical usage, they have distinct meanings: "anxiety" is defined as an unpleasant emotional state for which the cause is either not readily identified or perceived to be uncontrollable or unavoidable, whereas "fear" is an emotional and physiological response to a recognized external threat.[68] The term "anxiety disorder" includes fears (phobias) as well as anxieties.
The diagnosis of anxiety disorders is difficult because there are no objective biomarkers, it is based on symptoms,[69] which typically need to be present at least six months, be more than would be expected for the situation, and decrease functioning.[2][4] Several generic anxiety questionnaires can be used to detect anxiety symptoms, such as the State-Trait Anxiety Inventory (STAI), the Generalized Anxiety Disorder 7 (GAD-7), the Beck Anxiety Inventory (BAI), the Zung Self-Rating Anxiety Scale, and the Taylor Manifest Anxiety Scale.[70] Other questionnaires combine anxiety and depression measurement, such as the Hamilton Anxiety Rating Scale, the Hospital Anxiety and Depression Scale (HADS), the Patient Health Questionnaire (PHQ), and the Patient-Reported Outcomes Measurement Information System (PROMIS).[70] Examples of specific anxiety questionnaires include the Liebowitz Social Anxiety Scale (LSAS), the Social Interaction Anxiety Scale (SIAS), the Social Phobia Inventory (SPIN), the Social Phobia Scale (SPS), and the Social Anxiety Questionnaire (SAQ-A30).[71]
Anxiety disorders often occur along with other mental disorders, in particular depression, which may occur in as many as 60% of people with anxiety disorders. The fact that there is considerable overlap between symptoms of anxiety and depression, and that the same environmental triggers can provoke symptoms in either condition, may help to explain this high rate of comorbidity.[72]
Studies have also indicated that anxiety disorders are more likely among those with family history of anxiety disorders, especially certain types.[73]
Sexual dysfunction often accompanies anxiety disorders, although it is difficult to determine whether anxiety causes the sexual dysfunction or whether they arise from a common cause. The most common manifestations in individuals with anxiety disorder are avoidance of intercourse, premature ejaculation or erectile dysfunction among men and pain during intercourse among women. Sexual dysfunction is particularly common among people affected by panic disorder (who may fear that a panic attack will occur during sexual arousal) and posttraumatic stress disorder.[74]
Differential diagnosis
The diagnosis of an anxiety disorder requires first ruling out an underlying medical cause.[5][68] Diseases that may present similar to an anxiety disorder, including certain endocrine diseases (hypo- and hyperthyroidism, hyperprolactinemia),[68][4][5][75] metabolic disorders (diabetes),[5][76] deficiency states (low levels of vitamin D, B2, B12, folic acid),[5] gastrointestinal diseases (celiac disease, non-celiac gluten sensitivity, inflammatory bowel disease),[77][78][79] heart diseases,[4][5] blood diseases (anemia),[5] and brain degenerative diseases (Parkinson's disease, dementia, multiple sclerosis, Huntington's disease).[5][80][81][82]
Also, several drugs can cause or worsen anxiety, whether in intoxication, withdrawal, or from chronic use. These include alcohol, tobacco, cannabis, sedatives (including prescription benzodiazepines), opioids (including prescription pain killers and illicit drugs like heroin), stimulants (such as caffeine, cocaine and amphetamines), hallucinogens, and inhalants.[4][83]
Treatment
Treatment options include lifestyle changes, therapy, and medications. There is no good evidence as to whether therapy or medication is more effective; the choice of which is up to the person with the anxiety disorder and most choose therapy first.[84] The other may be offered in addition to the first choice or if the first choice fails to relieve symptoms.[84]
Lifestyle changes
Lifestyle changes include exercise, for which there is moderate evidence for some improvement, regularizing sleep patterns, reduce caffeine intake, and stopping smoking.[84] Stopping smoking has benefits in anxiety as large as or larger than those of medications.[85]
Therapy
Cognitive behavioral therapy (CBT) is effective for anxiety disorders and is a first line treatment.[84][86][87][88] CBT appears to be equally effective when carried out via the internet.[89] While evidence for mental health apps is promising it is preliminary.[90]
Self-help books can contribute to the treatment of people with anxiety disorders.[91]
Mindfulness based programs also appear to be effective for managing anxiety disorders.[92][93] It is unclear if meditation has an effect on anxiety and transcendental meditation appears to be no different than other types of meditation.[94]
Medications
Medications include SSRIs or SNRIs are first line choices for generalized anxiety disorder; there is no good evidence for any member of the class being better than another, so cost often drives drug choice.[84] Buspirone, quetiapine and pregabalin are second line treatments for people who do not respond to SSRIs or SNRIs; there is also evidence that benzodiazepines including diazepam and clonazepam are effective but these are not preferred due to the risk of dependence.[84]
Medications need to be used with care among older adults, who are more likely to have side effects because of coexisting physical disorders. Adherence problems are more likely among older people, who may have difficulty understanding, seeing, or remembering instructions.[8]
In general medications are not seen as helpful in specific phobia but a benzodiazepine is sometimes used to help resolve acute episodes; as 2007 data were sparse for efficacy of any drug.[95]
Alternative medicine
Many other remedies have been used for anxiety disorder. These include kava, where the potential for benefit seems greater than that for harm with short-term use in those with mild to moderate anxiety.[96][97] The American Academy of Family Physicians (AAFP) recommends use of kava for those with mild to moderate anxiety disorders who are not using alcohol or taking other medicines metabolized by the liver, but who wish to use "natural" remedies.[98] Side effects of kava in the clinical trials were rare and mild.
Inositol has been found to have modest effects in people with panic disorder or obsessive-compulsive disorder.[99] There is insufficient evidence to support the use of St. John's wort, valerian or passionflower.[99]
Aromatherapy has shown some tentative benefits for anxiety reduction in people with cancer when done with massages, although it not clear whether it could just enhance the effect of massage itself.[100]
Children
Several methods of treatment have been found to be effective in treating childhood anxiety disorders. Therapy is strongly preferred to medication.[101]
Cognitive behavioral therapy (CBT), a well-established treatment for anxiety related disorders in children and adolescents, is a good first therapy approach.[101] Studies have also gathered substantial evidence for treatments that are not CBT based as being effective forms of treament, expanding treatment options for those who do not respond to CBT.[101] Like adults, children may undergo psychotherapy, cognitive-behavioral therapy, or counseling. Family therapy is a form of treatment in which the child meets with a therapist together with the primary guardians and siblings. Each family member may attend individual therapy, but family therapy is typically a form of group therapy. Art and play therapy are also used. Art therapy is most commonly used when the child will not or cannot verbally communicate, due to trauma or a disability in which they are nonverbal. Participating in art activities allows the child to express what they otherwise may not be able to communicate to others.[102] In play therapy, the child is allowed to play however they please as a therapist observes them. The therapist may intercede from time to time with a question, comment, or suggestion. This is often most effective when the family of the child plays a significant role in the treatment.[103]
In children and adolescents, a medication option is warranted, antidepressants such as SSRIs, SNRIs as well as tricyclic antidepressants can be effective.[104]
Prognosis
The prognosis varies on the severity of each case and utilization of treatment for each individual. [105]
If these children are left untreated, they face risks such as poor results at school, avoidance of important social activities, and substance abuse. Children who have an anxiety disorder are likely to have other disorders such as depression, eating disorders, attention deficit disorders both hyperactive and inattentive.
Epidemiology
Globally as of 2010 approximately 273 million (4.5% of the population) had an anxiety disorder.[106] It is more common in females (5.2%) than males (2.8%).[106]
In Europe, Africa and Asia, lifetime rates of anxiety disorders are between 9 and 16%, and yearly rates are between 4 and 7%.[107] In the United States, the lifetime prevalence of anxiety disorders is about 29%[108] and between 11 and 18% of adults have the condition in a given year.[107] This difference is affected by the range of ways in which different cultures interpret anxiety symptoms and what they consider to be normative behavior.[109][110] In general, anxiety disorders represent the most prevalent psychiatric condition in the United States, outside of substance use disorder.[111]
Children
Like adults, children can experience anxiety disorders; between 10 and 20 percent of all children will develop a full-fledged anxiety disorder prior to the age of 18,[112] making anxiety the most common mental health issue in young people. Anxiety disorders in children are often more challenging to identify than their adult counterparts owing to the difficulty many parents face in discerning them from normal childhood fears. Likewise, anxiety in children is sometimes misdiagnosed as an attention deficit disorder or, due to the tendency of children to interpret their emotions physically (as stomach aches, head aches, etc.), anxiety disorders may initially be confused with physical ailments.[113]
Anxiety in children has a variety of causes; sometimes anxiety is rooted in biology, and may be a product of another existing condition, such as Autism or Asperger's Disorder.[114] Gifted children are also often more prone to excessive anxiety than non-gifted children.[115] Other cases of anxiety arise from the child having experienced a traumatic event of some kind, and in some cases, the cause of the child's anxiety cannot be pinpointed.[116]
Anxiety in children tends to manifest along age-appropriate themes, such as fear of going to school (not related to bullying) or not performing well enough at school, fear of social rejection, fear of something happening to loved ones, etc. What separates disordered anxiety from normal childhood anxiety is the duration and intensity of the fears involved.[113]
A small child will usually experience separation anxiety, for example, but he or she will generally grow out of it by about the age of 6, whereas in an anxious child it may linger for years longer, hindering the child's development.[117] Similarly, most children will fear the dark or losing their parents at some point, but this fear will dissipate over time without interfering a great deal in that child's normal day-to-day activities. In a child with an anxiety disorder, fearing the dark or loss of loved ones may grow into a lasting obsession which the child tries to deal with in compulsive ways which erode his or her quality of life.[117] The presence of co- occurring depressive symptoms in anxiety disorders may mark the transition to a more severe and detrimental and impairing disorder in preschool and early school age.[118]
Children, similar to adults, may suffer from a range of different anxiety disorders, including:
Generalized anxiety disorder: The child experiences persistent anxiety regarding a wide variety of situations, and this anxiety may adapt to fit each new situation that arises or be based largely on imagined situations which have yet to occur. Reassurance often has little effect.[113][117]
Separation anxiety disorder: A child who is older than 6 or 7 who has an extremely difficult time being away from his or her parents may be experiencing Separation Anxiety Disorder. Children with this disorder often fear that they will lose their loved ones during times of absence. As such, they frequently refuse to attend school.[119]
Social anxiety disorder should not be confused with shyness or introversion; shyness is frequently normal, especially in very young children. Children with social anxiety disorder often wish to engage in social activity (unlike introverts) but find themselves held back by obsessive fears of being disliked. They often convince themselves they have made a poor impression on others, regardless of evidence to the contrary. Over time, they may develop a phobia of social situations.[120] This disorder affects older children and preteens more often than younger children. Social phobia in children may also be caused by some traumatic event, such as not knowing an answer when called on in class.[121]
While uncommon in children, OCD can occur. Rates are between two and four percent.[122] Like adults, children rely on "magical thinking" in order to allay their anxiety, i.e., he or she must perform certain rituals (often based in counting, organizing, cleaning, etc.) in order to "prevent" the calamity he or she feels is imminent. Unlike normal children, who can leave their magical thinking-based activities behind when called upon to do so, children with OCD are literally unable to cease engaging in these activities, regardless of the consequences.[117][123]
Panic disorder is more common in older children, though younger children sometimes also suffer from it. Panic disorder is frequently mistaken for a physical illness by children suffering from it, likely due to its strongly physical symptoms (a racing heartbeat, sweating, dizziness, nausea, etc.) These symptoms are, however, usually accompanied by extreme fear, particularly the fear of dying. Like adults with Panic Disorder, children may attempt to avoid any situation they feel is a "trigger" for their attacks.[117]
References
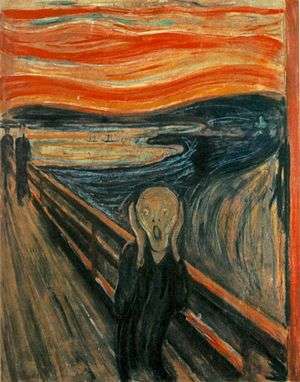
- ↑ Peter Aspden (21 April 2012). "So, what does 'The Scream' mean?". Financial Times.
- 1 2 3 4 5 6 Diagnostic and Statistical Manual of Mental DisordersAmerican Psychiatric Associati. (5th ed.). Arlington: American Psychiatric Publishing. 2013. pp. 189–195. ISBN 978-0890425558.
- 1 2 3 "Anxiety Disorders". NIMH. March 2016. Retrieved 14 August 2016.
- 1 2 3 4 5 6 7 8 9 10 11 Craske, MG; Stein, MB (24 June 2016). "Anxiety.". Lancet (London, England). PMID 27349358.
- 1 2 3 4 5 6 7 8 Testa A, Giannuzzi R, Daini S, Bernardini L, Petrongolo L, Gentiloni Silveri N (2013). "Psychiatric emergencies (part III): psychiatric symptoms resulting from organic diseases" (PDF). Eur Rev Med Pharmacol Sci (Review). 17 Suppl 1: 86–99. PMID 23436670.

- ↑ Kessler; et al. (2007). "Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health Organization's World Mental Health Survey Initiative". World Psychiatry. 6 (3): 168–76. PMID 18188442.
- ↑ Schacter, D. L., Gilbert, D. T., & Wegner, D.M. (2011). Psychology: Second Edition. New York, NY: Worth.
- 1 2 3 Calleo J, Stanley M (2008). "Anxiety Disorders in Later Life: Differentiated Diagnosis and Treatment Strategies". Psychiatric Times. 26 (8).
- 1 2 3 Phil Barker (7 October 2003). Psychiatric and mental health nursing: the craft of caring. London: Arnold. ISBN 978-0-340-81026-2. Retrieved 17 December 2010.
- ↑ Psychology, Michael Passer, Ronald Smith, Nigel Holt, Andy Bremner, Ed Sutherland, Michael Vliek (2009) McGrath Hill Education, UK: McGrath Hill Companies Inc. p 790
- ↑ http://www.webmd.com/anxiety-panic/guide/mental-health-anxiety-disorders
- ↑ Psychiatry, Michael Gelder, Richard Mayou, John Geddes 3rd ed. Oxford; New York: Oxford University Press, c 2005 p. 75
- ↑ Varcarolis. E (2010). Manual of Psychiatric Nursing Care Planning: Assessment Guides, Diagnoses and Psychopharmacology. 4th ed. New York: Saunders Elsevier. p 109.
- 1 2 Keeton, CP; Kolos, AC; Walkup, JT (2009). "Pediatric generalized anxiety disorder: epidemiology, diagnosis, and management.". Paediatric drugs. 11 (3): 171–83. doi:10.2165/00148581-200911030-00003. PMID 19445546.
- ↑ Psychology. Michael Passer, Ronald Smith, Nigel Holt, Andy Bremner, Ed Sutherland, Michael Vliek. (2009) McGrath Hill Higher Education; UK: McGrath Hill companies Inc.
- ↑ "Panic Disorder". Center for the Treatment and Study of Anxiety, University of Pennsylvania.
- ↑ Craske 2003 Gorman, 2000
- ↑ Jane E. Fisher; William T. O'Donohue (27 July 2006). Practitioner's Guide to Evidence-Based Psychotherapy. Springer. p. 754. ISBN 978-0387283692.
- ↑ The Oxford Handbook of Exercise Psychology. Oxford University Press. 2012. p. 56. ISBN 9780199930746.
- ↑ Post-Traumatic Stress Disorder and the Family. Veterans Affairs Canada. 2006. ISBN 0-662-42627-4.
- ↑ Psychological Disorders, Psychologie Anglophone
- ↑ Fullerton, Carol (1997). Posttraumatic Stress Disorder. Washington, D.C.: American Psychiatric Press Inc. pp. 8–9. ISBN 0-88048-751-8.
- ↑ Siegler, Robert (2006). How Children Develop, Exploring Child Develop Student Media Tool Kit & Scientific American Reader to Accompany How Children Develop. New York: Worth Publishers. ISBN 0-7167-6113-0.
- ↑ "Adult Separation Anxiety Often Overlooked Diagnosis – Arehart-Treichel 41 (13): 30 – Psychiatr News". Psychiatric News. Retrieved 20 February 2012.
- ↑ Shear, K.; Jin, R.; Ruscio, AM.; Walters, EE.; Kessler, RC. (June 2006). "Prevalence and correlates of estimated DSM-IV child and adult separation anxiety disorder in the National Comorbidity Survey Replication". Am J Psychiatry. 163 (6): 1074–1083. doi:10.1176/appi.ajp.163.6.1074. PMC 1924723
 . PMID 16741209.
. PMID 16741209. - ↑ Mohatt, Justin; Bennett, Shannon M.; Walkup, John T. (2014-07-01). "Treatment of Separation, Generalized, and Social Anxiety Disorders in Youths". American Journal of Psychiatry. 171 (7): 741–748. doi:10.1176/appi.ajp.2014.13101337. ISSN 0002-953X.
- ↑ Situational Panic Attacks. (n.d.). Retrieved from http://www.sound-mind.org/situational-panic-attacks.html
- 1 2 3 4 National Collaborating Centre for Mental Health, (UK) (2006). "Obsessive-Compulsive Disorder: Core Interventions in the Treatment of Obsessive-Compulsive Disorder and Body Dysmorphic Disorder,". NICE Clinical Guidelines (31). PMID 21834191. Retrieved 21 November 2015.
- 1 2 3 4 5 Soomro, GM (18 January 2012). "Obsessive compulsive disorder.". BMJ clinical evidence. 2012. PMC 3285220
 . PMID 22305974.
. PMID 22305974. - 1 2 Institute for Quality and Efficiency in Health Care (IQWiG). "Obsessive-compulsive disorder: overview". PubMed Health. Institute for Quality and Efficiency in Health Care (IQWiG). Retrieved 21 November 2015.
- ↑ Evans, Katie; Sullivan, Michael J. (1 March 2001). Dual Diagnosis: Counseling the Mentally Ill Substance Abuser (2nd ed.). Guilford Press. pp. 75–76. ISBN 978-1-57230-446-8.
- ↑ Lindsay, S.J.E.; Powell, Graham E., eds. (28 July 1998). The Handbook of Clinical Adult Psychology (2nd ed.). Routledge. pp. 152–153. ISBN 978-0-415-07215-1.
- ↑ Johnson, Bankole A. (2011). Addiction medicine : science and practice. New York: Springer. pp. 301–303. ISBN 978-1-4419-0337-2.
- ↑ Cohen SI (February 1995). "Alcohol and benzodiazepines generate anxiety, panic and phobias". J R Soc Med. 88 (2): 73–77. PMC 1295099
 . PMID 7769598.
. PMID 7769598. - ↑ Morrow LA; et al. (2000). "Increased incidence of anxiety and depressive disorders in persons with organic solvent exposure". Psychosomat Med. 62 (6): 746–750. doi:10.1097/00006842-200011000-00002. PMID 11138992.
- ↑ Scott, Trudy (2011). The Antianxiety Food Solution: How the Foods You Eat Can Help You Calm Your Anxious Mind, Improve Your Mood, and End Cravings. New Harbinger Publications. p. 59. ISBN 1-57224-926-9. Retrieved 7 October 2012.
- ↑ Winston AP (2005). "Neuropsychiatric effects of caffeine". Advances in Psychiatric Treatment. 11 (6): 432–439. doi:10.1192/apt.11.6.432.
- ↑ Hughes RN (June 1996). "Drugs Which Induce Anxiety: Caffeine". New Zealand Journal of Psychology. 25 (1): 36–42.
- ↑ Vilarim MM, Rocha Araujo DM, Nardi AE (August 2011). "Caffeine challenge test and panic disorder: a systematic literature review". Expert Rev Neurother. 11 (8): 1185–95. doi:10.1586/ern.11.83. PMID 21797659.
- ↑ Vilarim, Marina Machado; Rocha Araujo, Daniele Marano; Nardi, Antonio Egidio (2011). "Caffeine challenge test and panic disorder: A systematic literature review". Expert Review of Neurotherapeutics. 11 (8): 1185–95. doi:10.1586/ern.11.83. PMID 21797659.
- ↑ Bruce, Malcolm; Scott, N; Shine, P; Lader, M (1992). "Anxiogenic Effects of Caffeine in Patients with Anxiety Disorders". Archives of General Psychiatry. 49 (11): 867–9. doi:10.1001/archpsyc.1992.01820110031004. PMID 1444724.
- ↑ Nardi, Antonio E.; Lopes, Fabiana L.; Valença, Alexandre M.; Freire, Rafael C.; Veras, André B.; De-Melo-Neto, Valfrido L.; Nascimento, Isabella; King, Anna Lucia; Mezzasalma, Marco A.; Soares-Filho, Gastão L.; Zin, Walter A. (2007). "Caffeine challenge test in panic disorder and depression with panic attacks". Comprehensive Psychiatry. 48 (3): 257–63. doi:10.1016/j.comppsych.2006.12.001. PMID 17445520.
- ↑ American Psychiatric Association (2013). Diagnostic and Statistical Manual of Mental Disorders (DSM-5). American Psychiatric Publishing. pp. 226–230. ISBN 978-0-89042-555-8.
- ↑ Kedzior, Karina Karolina; Laeber, Lisa Tabata (2014-05-10). "A positive association between anxiety disorders and cannabis use or cannabis use disorders in the general population- a meta-analysis of 31 studies". BMC Psychiatry. 14: 136. doi:10.1186/1471-244X-14-136. ISSN 1471-244X. PMC 4032500
 . PMID 24884989.
. PMID 24884989. - ↑ Crippa, José Alexandre; Zuardi, Antonio Waldo; Martín-Santos, Rocio; Bhattacharyya, Sagnik; Atakan, Zerrin; McGuire, Philip; Fusar-Poli, Paolo (2009-10-01). "Cannabis and anxiety: a critical review of the evidence". Human Psychopharmacology: Clinical and Experimental. 24 (7): 515–523. doi:10.1002/hup.1048. ISSN 1099-1077. PMID 19693792.
- ↑ Kantorovich V, Eisenhofer G, Pacak K (2008). "Pheochromocytoma: an endocrine stress mimicking disorder". Ann. N. Y. Acad. Sci. 1148: 462–8. doi:10.1196/annals.1410.081. PMC 2693284
 . PMID 19120142.
. PMID 19120142. - ↑ Guller U, Turek J, Eubanks S, Delong ER, Oertli D, Feldman JM (2006). "Detecting pheochromocytoma: defining the most sensitive test". Ann. Surg. 243: 102–7. doi:10.1097/01.sla.0000193833.51108.24. PMC 1449983
 . PMID 16371743.
. PMID 16371743. - ↑ http://www.medscape.com/viewarticle/723663_6
- ↑ Patel, G; Fancher, TL (3 Dec 2013). "In the clinic. Generalized anxiety disorder.". Annals of Internal Medicine. 159 (11): ITC6–1, ITC6–2, ITC6–3, ITC6–4, ITC6–5, ITC6–6, ITC6–7, ITC6–8, ITC6–9, ITC6–10, ITC6–11; quiz ITC6–12. doi:10.7326/0003-4819-159-11-201312030-01006. PMID 24297210.
- 1 2 3 Grinde, B (2005). "An approach to the prevention of anxiety-related disorders based on evolutionary medicine" (PDF). Preventative Medicine. 40 (6): 904–909. doi:10.1016/j.ypmed.2004.08.001. PMID 15850894.
- 1 2 3 Bateson, M; B. Brilot; D. Nettle (2011). "Anxiety: An evolutionary approach" (PDF). Canadian Journal of Psychiatry. 56 (12): 707–715.
- 1 2 Price, John S. (September 2003). "Evolutionary aspects of anxiety disorders". Dialogues in Clinical Neuroscience. 5 (3): 223–236. PMC 3181631
 . PMID 22033473.
. PMID 22033473. - ↑ Lydiard RB (2003). "The role of GABA in anxiety disorders". J Clin Psychiatry. 64 (Suppl 3): 21–27. PMID 12662130.
- ↑ Nemeroff CB (2003). "The role of GABA in the pathophysiology and treatment of anxiety disorders". Psychopharmacol Bull. 37 (4): 133–146. PMID 15131523.
- ↑ Enna SJ (1984). "Role of gamma-aminobutyric acid in anxiety". Psychopathology. 17 (Suppl 1): 15–24. doi:10.1159/000284073. PMID 6143341.
- ↑ Dunlop BW, Davis PG (2008). "Combination treatment with benzodiazepines and SSRIs for comorbid anxiety and depression: a review". Prim Care Companion J Clin Psychiatry. 10 (3): 222–228. doi:10.4088/PCC.v10n0307. PMC 2446479
 . PMID 18615162.
. PMID 18615162. - 1 2 3 Etkin A, Prater KE, Schatzberg AF, Menon V, Greicius MD (2009). "Disrupted amygdalar subregion functional connectivity and evidence of a compensatory network in generalized anxiety disorder". Arch Gen Psychiatry. 66 (12): 1361–1372. doi:10.1001/archgenpsychiatry.2009.104. PMID 19996041.
- ↑ Kalueff AV, Ishikawa K, Griffith AJ (10 January 2008). "Anxiety and otovestibular disorders: linking behavioral phenotypes in men and mice". Behav. Brain Res. 186 (1): 1–11. doi:10.1016/j.bbr.2007.07.032. PMID 17822783.
- ↑ Nagaratnam N, Ip J, Bou-Haidar P (May–June 2005). "The vestibular dysfunction and anxiety disorder interface: a descriptive study with special reference to the elderly". Arch Gerontol Geriatr. 40 (3): 253–264. doi:10.1016/j.archger.2004.09.006. PMID 15814159.
- ↑ Lepicard EM, Venault P, Perez-Diaz F, Joubert C, Berthoz A, Chapouthier G (20 December 2000). "Balance control and posture differences in the anxious BALB/cByJ mice compared to the non anxious C57BL/6J mice". Behav. Brain Res. 117 (1–2): 185–195. doi:10.1016/S0166-4328(00)00304-1. PMID 11099772.
- ↑ Simon NM, Pollack MH, Tuby KS, Stern TA (June 1998). "Dizziness and panic disorder: a review of the association between vestibular dysfunction and anxiety". Ann Clin Psychiatry. 10 (2): 75–80. doi:10.3109/10401239809147746. PMID 9669539.
- ↑ Balaban CD, Thayer JF (January–April 2001). "Neurological bases for balance-anxiety links". J Anxiety Disord. 15 (1–2): 53–79. doi:10.1016/S0887-6185(00)00042-6. PMID 11388358.
- ↑ Mitra R, Ferguson D, Sapolsky RM (10 February 2009). "SK2 potassium channel overexpression in basolateral amygdala reduces anxiety, stress-induced corticosterone secretion and dendritic arborization". Mol. Psychiatry. 14 (9): 847–855, 827. doi:10.1038/mp.2009.9. PMC 2763614
 . PMID 19204724.
. PMID 19204724. - 1 2 Bienvenu, OJ; Ginsburg, GS (December 2007). "Prevention of anxiety disorders". International review of psychiatry (Abingdon, England). 19 (6): 647–54. doi:10.1080/09540260701797837. PMID 18092242.
- ↑ Khoury B, Lecomte T, Fortin G, et al. (Aug 2013). "Mindfulness-based therapy: a comprehensive meta-analysis". Clin Psychol Rev. 33 (6): 763–71.
- ↑ Sharma M, Rush SE (Jul 2014). "Mindfulness-based stress reduction as a stress management intervention for healthy individuals: a systematic review". J Evid Based Complementary Altern Med. 19 (4): 271–86. doi:10.1177/2156587214543143. PMID 25053754.
- ↑ Patel, G; Fancher, TL (3 December 2013). "In the clinic. Generalized anxiety disorder." (PDF). Annals of Internal Medicine. 159 (11): ITC6–1, ITC6–2, ITC6–3, ITC6–4, ITC6–5, ITC6–6, ITC6–7, ITC6–8, ITC6–9, ITC6–10, ITC6–11; quiz ITC6–12. doi:10.7326/0003-4819-159-11-201312030-01006. PMID 24297210.
currently there is no evidence on the effectiveness of preventive measures for GAD in adult
- 1 2 3 World Health Organization (2009). Pharmacological Treatment of Mental Disorders in Primary Health Care (PDF). Geneva. ISBN 978-92-4-154769-7.
- ↑ Rose M, Devine J (2014). "Assessment of patient-reported symptoms of anxiety". Dialogues Clin Neurosci (Review). 16 (2): 197–211 (Table 1). PMC 4140513
 . PMID 25152658.
. PMID 25152658.
- 1 2 Rose M, Devine J (2014). "Assessment of patient-reported symptoms of anxiety". Dialogues Clin Neurosci (Review). 16 (2): 197–211 (Table 1). PMC 4140513
 . PMID 25152658.
. PMID 25152658.
- ↑ Rose M, Devine J (2014). "Assessment of patient-reported symptoms of anxiety". Dialogues Clin Neurosci (Review). 16 (2): 197–211 (Table 2). PMC 4140513
 . PMID 25152658.
. PMID 25152658.
- ↑ Cameron OG (1 December 2007). "Understanding Comorbid Depression and Anxiety". Psychiatric Times. 24 (14).
- ↑ McLaughlin K; Behar E; Borkovec T (25 August 2005). "Family history of psychological problems in generalized anxiety disorder". Journal of Clinical Psychology. 64 (7): 905–918. doi:10.1002/jclp.20497. PMID 18509873.
- ↑ Coretti G, Baldi I (1 August 2007). "The Relationship Between Anxiety Disorders and Sexual Dysfunction". Psychiatric Times. 24 (9).
- ↑ Samuels MH (2008). "Cognitive function in untreated hypothyroidism and hyperthyroidism". Curr Opin Endocrinol Diabetes Obes (Review). 15 (5): 429–33. doi:10.1097/MED.0b013e32830eb84c. PMID 18769215.
- ↑ Grigsby AB, Anderson RJ, Freedland KE, Clouse RE, Lustman PJ (2002). "Prevalence of anxiety in adults with diabetes: a systematic review". J Psychosom Res (Systematic Review). 53 (6): 1053–60. PMID 12479986.
- ↑ Zingone F, Swift GL, Card TR, Sanders DS, Ludvigsson JF, Bai JC (Apr 2015). "Psychological morbidity of celiac disease: A review of the literature". United European Gastroenterol J (Review). 3 (2): 136–45. doi:10.1177/2050640614560786. PMC 4406898
 . PMID 25922673.
. PMID 25922673. - ↑ Molina-Infante J, Santolaria S, Sanders DS, Fernández-Bañares F (May 2015). "Systematic review: noncoeliac gluten sensitivity". Aliment Pharmacol Ther (Systematic Review). 41 (9): 807–20. doi:10.1111/apt.13155. PMID 25753138.
- ↑ Neuendorf R, Harding A, Stello N, Hanes D, Wahbeh H (2016). "Depression and anxiety in patients with Inflammatory Bowel Disease: A systematic review". J Psychosom Res (Systematic Review). 87: 70–80. doi:10.1016/j.jpsychores.2016.06.001. PMID 27411754.
- ↑ Zhao QF, Tan L, Wang HF, Jiang T, Tan MS, Tan L, et al. (2016). "The prevalence of neuropsychiatric symptoms in Alzheimer's disease: Systematic review and meta-analysis". J Affect Disord (Systematic Review). 190: 264–71. PMID 26540080.
- ↑ Wen MC, Chan LL, Tan LC, Tan EK (2016). "Depression, anxiety, and apathy in Parkinson's disease: insights from neuroimaging studies". Eur J Neurol (Review). 23 (6): 1001–19. doi:10.1111/ene.13002. PMC 5084819
 . PMID 27141858.
. PMID 27141858. - ↑ Marrie RA, Reingold S, Cohen J, Stuve O, Trojano M, Sorensen PS, et al. (2015). "The incidence and prevalence of psychiatric disorders in multiple sclerosis: a systematic review". Mult Scler (Systematic Review). 21 (3): 305–17. doi:10.1177/1352458514564487. PMC 4429164
 . PMID 25583845.
. PMID 25583845. - ↑ American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders, fifth edition. Arlington, VA: American Psychiatric Association. ISBN 978-0890425558.
- 1 2 3 4 5 6 Stein, MB; Sareen, J (19 November 2015). "Clinical Practice: Generalized Anxiety Disorder.". The New England journal of medicine. 373 (21): 2059–68. PMID 26580998.
- ↑ Taylor, G.; McNeill, A.; Girling, A.; Farley, A.; Lindson-Hawley, N.; Aveyard, P. (13 February 2014). "Change in mental health after smoking cessation: systematic review and meta-analysis". BMJ. 348 (feb13 1): g1151–g1151. doi:10.1136/bmj.g1151. PMC 3923980
 . PMID 24524926.
. PMID 24524926. - ↑ Cuijpers, P; Sijbrandij, M; Koole, S; Huibers, M; Berking, M; Andersson, G (Mar 2014). "Psychological treatment of generalized anxiety disorder: A meta-analysis.". Clinical Psychology Review. 34 (2): 130–140. doi:10.1016/j.cpr.2014.01.002. PMID 24487344.
- ↑ Otte, C (2011). "Cognitive behavioral therapy in anxiety disorders: current state of the evidence.". Dialogues in clinical neuroscience. 13 (4): 413–21. PMC 3263389
 . PMID 22275847.
. PMID 22275847. - ↑ Pompoli, A; Furukawa, TA; Imai, H; Tajika, A; Efthimiou, O; Salanti, G (13 April 2016). "Psychological therapies for panic disorder with or without agoraphobia in adults: a network meta-analysis.". The Cochrane database of systematic reviews. 4: CD011004. PMID 27071857.
- ↑ Olthuis, JV; Watt, MC; Bailey, K; Hayden, JA; Stewart, SH (12 March 2016). "Therapist-supported Internet cognitive behavioural therapy for anxiety disorders in adults.". The Cochrane database of systematic reviews. 3: CD011565. PMID 26968204.
- ↑ Donker, T; Petrie, K; Proudfoot, J; Clarke, J; Birch, MR; Christensen, H (15 November 2013). "Smartphones for smarter delivery of mental health programs: a systematic review.". Journal of medical Internet research. 15 (11): e247. doi:10.2196/jmir.2791. PMC 3841358
 . PMID 24240579.
. PMID 24240579. - ↑ Warren Mansell (1 June 2007). "Reading about self-help books on cognitive-behavioural therapy for anxiety disorders". Pb.rcpsych.org. Retrieved 20 February 2012.
- ↑ Roemer L, Williston SK, Eustis EH (Nov 2013). "Mindfulness and acceptance-based behavioral therapies for anxiety disorders". Curr Psychiatry Rep. 15 (11): 410. doi:10.1007/s11920-013-0410-3.
- ↑ Lang AJ (May 2013). "What mindfulness brings to psychotherapy for anxiety and depression". Depress Anxiety. 30 (5): 409–12. doi:10.1002/da.22081.
- ↑ Krisanaprakornkit, T; Krisanaprakornkit, W; Piyavhatkul, N; Laopaiboon, M (25 January 2006). "Meditation therapy for anxiety disorders.". The Cochrane database of systematic reviews (1): CD004998. doi:10.1002/14651858.CD004998.pub2. PMID 16437509.
- ↑ Choy, Y; Fyer, AJ; Lipsitz, JD (April 2007). "Treatment of specific phobia in adults.". Clinical psychology review. 27 (3): 266–86. PMID 17112646.
- ↑ Pittler MH, Ernst E (2003). Pittler MH, ed. "Kava extract for treating anxiety". Cochrane Database of Systematic Reviews (1): CD003383. doi:10.1002/14651858.CD003383. PMID 12535473.
- ↑ Witte S, Loew D, Gaus W (March 2005). "Meta-analysis of the efficacy of the acetonic kava-kava extract WS1490 in patients with non-psychotic anxiety disorders". Phytother Res. 19 (3): 183–188. doi:10.1002/ptr.1609. PMID 15934028.
- ↑ Saeed SA, Bloch RM, Antonacci DJ (August 2007). "Herbal and dietary supplements for treatment of anxiety disorders". Am Fam Physician. 76 (4): 549–556. PMID 17853630.
- 1 2 Saeed, SA; Bloch, RM; Antonacci, DJ (15 Aug 2007). "Herbal and dietary supplements for treatment of anxiety disorders". American family physician. 76 (4): 549–56. PMID 17853630.
- ↑ Fellowes, D.; Barnes, K.; Wilkinson, S. (2004-01-01). "Aromatherapy and massage for symptom relief in patients with cancer". The Cochrane Database of Systematic Reviews (2): CD002287. doi:10.1002/14651858.CD002287.pub2. ISSN 1469-493X. PMID 15106172.
- 1 2 3 Higa-McMillan, CK; Francis, SE; Rith-Najarian, L; Chorpita, BF (18 June 2015). "Evidence Base Update: 50 Years of Research on Treatment for Child and Adolescent Anxiety.". Journal of Clinical Child and Adolescent Psychology: 1–23. doi:10.1080/15374416.2015.1046177. PMID 26087438.
- ↑ Kozlowska K.; Hanney L. (1999). "Family assessment and intervention using an interactive are exercise". Australia and New Zealand Journal of Family Therapy. 20 (2): 61–69. doi:10.1002/j.1467-8438.1999.tb00358.x.
- ↑ Bratton, S.C., & Ray, D. (2002). Humanistic play therapy. In D.J. Cain (Ed.), Humanistic psychotherapies: Handbook of research and practice (pp. 369-402). Washington, DC: American Psychological Association.
- ↑ Social Phobia at eMedicine
- ↑ Stanford University School of Medicine, Department of Psychiatry and Behavioral Sciences. "Principles and Practice of Geriatric Psychology, Second Edition". Principles and Practice of Geriatric Psychiatry. Pamela J. Swales, Erin L. Cassidy. Javaid I. Sheikh: 555–557. doi:10.1002/0470846410.ch101. Retrieved 13 February 2012.
- 1 2 Vos, T; Flaxman, AD; Naghavi, M; Lozano, R; Michaud, C; Ezzati, M; Shibuya, K; Salomon, JA; Abdalla, S; et al. (15 Dec 2012). "Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010". Lancet. 380 (9859): 2163–96. doi:10.1016/S0140-6736(12)61729-2. PMID 23245607.
- 1 2 Simpson, Helen Blair, ed. (2010). Anxiety disorders : theory, research, and clinical perspectives (1. publ. ed.). Cambridge, UK: Cambridge University Press. p. 7. ISBN 978-0-521-51557-3.
- ↑ Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE (June 2005). "Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication". Arch. Gen. Psychiatry. 62 (6): 593–602. doi:10.1001/archpsyc.62.6.593. PMID 15939837.
- ↑ Brockveld, Kelia C.; Perini, Sarah J.; Rapee, Ronald M. (2014). "6". In Hofmann, Stefan G.; DiBartolo, Patricia M. Social Anxiety: Clinical, Developmental, and Social Perspectives (3 ed.). Elsevier. ISBN 978-0-12-394427-6.
- ↑ Hofmann, Stefan G.; Asnaani, Anu (December 2010). "Cultural Aspects in Social Anxiety and Social Anxiety Disorder". Depress Anxiety. 27 (12): 1117–1127. doi:10.1002/da.20759. PMC 3075954
 . PMID 21132847.
. PMID 21132847. - ↑ Fricchione, Gregory (12 August 2004). "Generalized Anxiety Disorder". New England Journal of Medicine. 351 (7): 675–682. doi:10.1056/NEJMcp022342.
- ↑ Essau, Cecilia A. (2006). Child and Adolescent Psychopathology: Theoretical and Clinical Implications. 27 church road, Hove, East Sussex: Routledge. p. 79.
- 1 2 3 AnxietyBC. "GENERALIZED ANXIETY". AnxietyBC. AnxietyBC. Retrieved 11 June 2015.
- ↑ Merrill, Anna. "Anxiety and Autism Spectrum Disorders". Indiana Resource Center for Autism. Indiana Resource Center for Autism. Retrieved 10 June 2015.
- ↑ Guignard, Jacques-Henri; Jacquet, Anne-Yvonne; Lubart, Todd I. "Perfectionism and Anxiety: A Paradox in Intellectual Giftedness?". PLOS. PLOS. Retrieved 10 June 2015.
- ↑ Rapee, Ronald M.; Schniering, Carolyn A.; Hudson, Jennifer L. "Anxiety Disorders During Childhood and Adolescence: Origins and Treatment" (PDF). Annual Review of Clinical Psychology.
- 1 2 3 4 5 Shenfield, Tali. "A Primer on Child and Adolescent Anxiety". Advanced Psychology.
- ↑ Klitzing K von, White LO, Otto Y, Fuchs S, Egger HL, Klein AM: Depressive comorbidity in preschool anxiety disorder. J Child Psychol Psychiatr 2014; 55: 1107–16.
- ↑ "Separation Anxiety in Children". WebMD. WebMD. Retrieved 11 June 2015.
- ↑ "SOCIAL ANXIETY DISORDER". AnxietyBC. AnxietyBC. Retrieved 11 June 2015.
- ↑ Biegel, D.E. (1995). Caregiver burden. In G.E. Maddox (Ed.), The encyclopedia of aging (2,d ed., pp. 138-141). New York: Springer
- ↑ Boileau, B (2011). "A review of obsessive-compulsive disorder in children and adolescents.". Dialogues in clinical neuroscience. 13 (4): 401–11. PMC 3263388
 . PMID 22275846.
. PMID 22275846. - ↑ Harvard Medical School (2004a). "December). Children's fears and anxieties". Harvard Mental Health Letter. 21 (6): 1–3.
Further reading
- Khouzam, HR (March 2009). "Anxiety Disorders: Guidelines for Effective Primary Care. Part 1: Diagnosis". Consultant. 49 (3).
- Khouzam, HR (April 2009). "Anxiety Disorders: Guidelines for Effective Primary Care. Part 2: Treatment". Consultant. 49 (4).
- Vanin, John; Helsley, James (2007). Anxiety Disorders: A Pocket Guide For Primary Care. Humana Press. ISBN 978-1-58829-923-9.
- Craske, Michelle Genevieve (2003). Origins of Phobias and Anxiety Disorders: Why More Women than Men?. Amsterdam: Elsevier. ISBN 0-08-044032-0.
- Schutz, Samantha (2006). I Don't Want to Be Crazy: A Memoir of Anxiety Disorder. www.samanthaschutz.net. PUSH. ISBN 978-0-439-80518-6.